A disease such as schizophrenic dementia is characterized by a decrease in intellectual abilities against the background of one of the forms of schizophrenia. Psychiatrists also call this disorder transient or apathetic dementia. The disease may be temporary, since there are no strong organic changes.
Characteristics of the disease
Dementia in schizophrenia is characterized by intellectual impairment and problems with perception. Nevertheless, it has been noted that many patients retain their acquired skills. The disease often does not affect memory. But a person stops using his knowledge because the motivation to do so disappears. In schizophrenia, the emotional sphere is disrupted. The patient has problems with such qualities as initiative, ingenuity, perseverance, and determination.
Intellectual abilities are negatively affected by the perception disorder characteristic of schizophrenia. The patient's thinking becomes ataxic. The constructions are grammatically constructed correctly, but contain nonsense and are illogical. Neologisms and cliches may slip into speech.
The memory of a patient with dementia, as with schizophrenia in general, remains intact. Such patients are well oriented in space and time. They remember what concerns their personality and environment.
Intellectual impairments in schizophrenia are temporary, as they depend on the emotional-volitional sphere of the patient.
General concept and characteristics
Schizophrenic dementia refers to the progressive degradation of mental abilities caused by any form of schizophrenia .
This pathology belongs to the category of unstable disorders, since at certain periods the patient may experience so-called “enlightenments”, during which his logical and thinking abilities are fully manifested.
Dementia as a result of dementia involves an irreversible change in the psyche, however, since with schizophrenia no organic or structural changes occur in the brain, the process proceeds in waves.
Currently, after a revision of medical names and criteria, dementia is combined with schizophrenia and can sometimes be called “dementia praecox” (dementia praecox), but this term is practically no longer used.
The fact is that the diagnosis of Dementia praecox, which began to be made at the end of the 19th century, has always referred to cases of the development of dementia in young men and adolescents.
But the symptoms of schizophrenia and dementia were in many ways similar, and gradually psychiatrists came to the conclusion that two different diseases have common symptoms , therefore, they should be combined in the international classification.
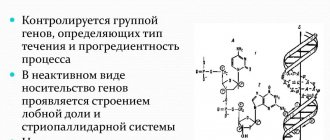
Pathogenesis
The pathogenesis of dementia in schizophrenia is not fully understood. But some scientists were interested in this issue. Thus, the Austrian psychiatrist J. Berze at the beginning of the 20th century called the disease “hypotension of consciousness.”
Despite the fact that in schizophrenia the intellect remains intact, its structure changes. This explains the main manifestations of the disease. The basis of schizophrenic dementia is the splitting of perception and intellect.
Causes of the appearance and development of the disease
The disease can occur after:
- receiving mechanical injuries of the skull and brain (TBI);
- tumors of the central nervous system;
- abuse of psychotropic and alcoholic substances;
- transmission of infectious diseases (AIDS, viral encephalitis, meningitis);
- severe liver or kidney failure;
- the presence of pathologies of the endocrine system;
- severe autoimmune diseases;
- establishing a diagnosis of diabetes mellitus and obesity.
Hereditary factors also play an important role in the manifestation of the disease. It is quite common for members of one family to suffer from dementia, especially in old age.
Causes
The causes of dementia are not fully known. But we can name factors that predispose to the development of the disease.
- Hormonal imbalances that can often be observed during adolescence;
- Heredity;
- Psychological defense mechanisms, including “displacement” of a stressful situation from consciousness, regression;
- Pathological changes in the brain;
- Drug intoxication, overdose of antipsychotic drugs.
Young women who have become mothers are often at risk. Emotional overload, hormonal imbalances, constant stress and lack of sleep are factors that provoke the development of the disease.
Classification of dementia
Taking into account the predominant damage to certain areas of the brain, four types of dementia are distinguished:
- Cortical dementia. The cerebral cortex is predominantly affected. It is observed in alcoholism, Alzheimer's disease and Pick's disease (frontotemporal dementia).
- Subcortical dementia. Subcortical structures suffer. Accompanied by neurological disorders (trembling limbs, muscle stiffness, gait disorders, etc.).
- Cortical-subcortical dementia. Both the cortex and subcortical structures are affected. Observed in vascular pathology.
- Multifocal dementia. Multiple areas of necrosis and degeneration form in various parts of the central nervous system. Neurological disorders are very diverse and depend on the location of the lesions.
Depending on the extent of the lesion, two forms of dementia are distinguished: total and lacunar.
- The high prevalence of dementia in the elderly led to the creation of a classification of senile dementias:
- Atrophic (Alzheimer's) type - provoked by primary degeneration of brain neurons.
- Vascular type - damage to nerve cells occurs secondary, due to disturbances in the blood supply to the brain due to vascular pathology.
- The mixed type - mixed dementia - is a combination of atrophic and vascular dementia.
Symptoms
Schizophrenic dementia is accompanied by symptoms such as:
- hallucinations and delusions;
- anxiety;
- a sharp change in emotional state, from strong excitement to lethargy;
- problems with orientation in space;
- panic attacks, the appearance of unreasonable fears;
- echolalia (repeating what is said after the interlocutor), etc.
Behavioral disturbances are temporary. A person may forget how to use household utensils (comb, cutlery, etc.), but the skills are soon restored. It is impossible to determine when the attack will begin and its duration.
Can it appear in children and young people?
What diseases can lead to dementia? In young and middle age, symptoms of acquired dementia can also be observed and there can be many reasons for this:
- Drug and alcohol addiction increases the risk of premature dementia.
- The presence of traumatic brain injuries, benign and malignant formations.
- The possibility of acquiring dementia praecox is also due to the presence of infectious diseases: chronic meningitis, viral encephalitis, AIDS, neurosyphilis.
Similar cases also affected patients with autoimmune diseases (systemic lupus erythematosus, multiple sclerosis), significant disturbances in the functioning of internal organs, and endocrine pathology (hormonal imbalances of the thyroid gland, Cushing's syndrome).
Diagnostics
The main method for diagnosing apathetic dementia is to collect anamnesis. First of all, close and relatives of the patient are interviewed, who can describe changes in his behavior. It is important to find out when the first symptoms of the disease appeared and how often they appear. Doctors also need to know whether the patient had relatives suffering from mental illness.
The following methods are used to assess the patient’s physical condition:
- blood chemistry;
- magnetic resonance imaging;
- electrocardiogram;
- diagnostic test for drug and psychoactive substance use.
Recommended. To assess the psychological state, standard methods with high relevance are recommended.
One of the most popular tests for diagnosing schizophrenic disorders is the Luscher color test. Its use is possible only if the patient’s cognitive functions are at least partially functioning. Patients are offered a short or full version of the test. It is believed that people suffering from dementia due to schizophrenia choose predominantly yellow and its shades.
Another effective diagnostic method is tracking a moving object. It is difficult for a person with schizophrenic disorder to keep their gaze on such an object. With apathetic dementia, the patient experiences problems with stability of attention.
Causes of dementia in schizophrenia
There is a debate among doctors about whether dementia in schizophrenia should be considered such at all. Since a person retains memory and general judgments, intelligence, only the manner of thinking changes.
A person suddenly begins to be afraid and hide. Emotions of fear arise from fantastic hallucinations. It can be assumed that the person was afraid of something. The cause of the exacerbation of the condition could be stress, some terrible event that occurred in a person’s life. Anxiety, depression, lack of understanding and love from others can lead to an exacerbation of the disease.
Treatment
The individual patient's condition influences the treatment of dementia in schizophrenia. For the disease, complex therapy is recommended. To reduce anxiety and fears, psychotherapy sessions are used, including hypnosis and relaxation. Individual consultations and group sessions are conducted with patients.
Depending on the symptoms that appear and their frequency, doctors prescribe medications. To maintain good shape, proper nutrition and physical activity are important. Treatment should be carried out under the supervision of a specialist who can note the effectiveness of the prescriptions and, if necessary, adjust the therapy.
Medicines
Schizophrenic dementia is treated in a hospital. Correct therapy can partially restore cognitive functions, but symptoms of schizophrenia can appear at any time. This disease cannot be treated without medication.
For schizophrenic dementia, the following groups of drugs can be prescribed:
- neuroleptic;
- nootropics;
- antidepressants;
- anxiolytics.
Neuroleptic drugs are prescribed to relieve attacks of delirium and hallucinations. Medicines are also used in maintenance therapy. Antipsychotics are aimed at psychotic disorders.
Nootropic drugs are recommended to restore cognitive functions. They are designed to stimulate anabolic processes in neurons, improve metabolism in nerve tissues, and cerebral blood flow. Antidepressants and anskiolytics have a calming effect, reduce anxiety, and relieve panic attacks.
Traditional methods
It is recommended to discuss the use of herbal tinctures and decoctions with your doctor. Tea with lemon balm and peppermint will help normalize sleep. Herbal decoctions have a calming effect, therefore they are recommended for high anxiety and excitability of the nervous system.
To normalize low blood pressure, it is recommended to take ginseng tincture. Decoctions of valerian and motherwort have calming properties.
Nutrition
A special menu for patients suffering from apathetic dementia is not required. But food should be high in calories and varied to maintain good physical shape. Fruits and vegetables, freshly squeezed juices will help restore a person’s self-control and lift their spirits.
The diet should include meat, nuts, and dairy products. The patient's menu should be thought out in such a way that it contains a sufficient amount of proteins, fats and carbohydrates. You should not include a lot of sweets in your diet, which can negatively affect the body's metabolism.
Exercises
A lot of time should be devoted to psychotherapy and establishing social connections for the patient. For schizophrenic dementia, sand and art therapy methods are recommended. Light physical activity and community service are also recommended for patients.
To restore cognitive functions, patients are offered tasks on attention, logic, and simple mathematical problems. Patients are recommended to play chess, solve riddles and puzzles.
Treatment regimen
At the moment, only medication is used to treat schizophrenic dementia, but it is considered only partially effective.
But in some cases, the patient’s cognitive abilities can be restored by 70-90%, although the symptoms of schizophrenic disorder do not disappear.
Treatment takes place in a hospital; antipsychotics are used as medications - drugs that affect the higher mental functions of the brain.
If the patient is in a highly agitated state, a course of antidepressants is prescribed . The secondary treatment is a psychological approach. It involves conversations with a specialist, group therapy and hypnosis sessions.
What should relatives do?
It is quite difficult for the loved ones of a person suffering from schizophrenic dementia, despite the fact that in most cases he can physically take care of himself. The main recommendations for relatives are as follows.
- Visit a psychotherapist. The specialist will talk about the peculiarities of communication with this disease and give recommendations for optimal behavior.
- The patient should be given physical and psychological stress to the best of his ability, and the range of responsibilities in everyday life should be determined.
- It is recommended to follow all doctor’s recommendations and monitor compliance with your daily routine. The patient must take walks in the fresh air, light physical activity, and good sleep.
- It is very important for relatives to provide the person with all possible help and attention in order to minimize his feelings of loneliness and anxiety.
Not recommended x Patients with schizophrenic dementia need to limit access to computer games and watching films, which can have a stimulating effect on the psyche.
Medical educational literature
Dementia (dementia) is an acquired mental defect with a predominant disorder of intellectual functions.
Signs of dementia are loss of accumulated abilities and knowledge, a general decrease in the productivity of mental activity, and personality changes. The dynamics of dementia vary. With brain tumors, atrophic diseases and atherosclerosis, mental defects constantly increase. In the case of post-traumatic and post-stroke dementia, restoration of some mental functions in the first months of the disease and a stable nature of symptoms over many subsequent years are possible. However, in general, the negative nature of dementia disorders determines its relative persistence and the impossibility of complete recovery.
The clinical picture of dementia differs significantly in the main mental illnesses - organic processes of epilepsy and schizophrenia.
Organic dementia is caused by a variety of diseases that lead to disruption of the structure of the brain and massive death of neurons.
The clinical picture of organic dementia is dominated by severe memory impairment and decreased ability to think abstractly. Presumably the cause of this syndrome can be judged by some features of the clinical picture of the disease. According to clinical manifestations, lacunar and total dementia are distinguished.
Lacunar (dysmnestic) dementia is manifested primarily by a memory disorder (the ability to form concepts and judgments is impaired much later).
This significantly complicates the ability to acquire new information, but professional knowledge and automated skills can be retained for a long time in such patients. Although they feel helpless in complex professional activities, they easily cope with daily household chores. Characteristically, there is a critical attitude towards their shortcomings: patients are embarrassed by their lack of independence, apologize for their sluggishness, and try (not always successfully) to compensate for memory impairment by writing down the most important thoughts on paper. Such patients are frank with the doctor, actively present complaints, and deeply experience their condition. Character changes in lacunar dementia are quite mild and do not affect the core of the personality. In general, relatives find that the basic forms of behavior, attachments, and beliefs of patients remain the same. However, more often than not, some sharpening of personality traits and a “caricature” of previous character traits are observed. Thus, frugality can turn into greed and stinginess, mistrust into suspicion, isolation into misanthropy. In the emotional sphere, patients with dysmnestic dementia are characterized by sentimentality, emotional lability, and tearfulness.
The cause of lacunar dementia is a variety of diffuse vascular diseases of the brain: non-stroke course of atherosclerosis and hypertension, diabetic microangiopathy, damage to systemic vessels due to collagenosis and syphilitic infection (lues cerebri). Changes in the state of the blood supply to the brain (improvement of the rheological properties of blood, taking vasodilators) can cause fluctuations in the condition and short periods of some improvement in these patients.
Total (global, paralytic) dementia is manifested by the primary loss of the ability to logic and understand reality.
Memory disorders can be very severe, but they can also lag significantly behind abstract thinking disorders. A sharp decrease or complete absence of a critical attitude towards the disease is noticeable. The pathological process often affects the moral properties of the individual: the sense of duty, delicacy, correctness, politeness, and modesty disappear. Personality disorders are so pronounced that patients cease to be like themselves (the “core of personality” is destroyed): they can cynically swear, expose themselves, urinate and defecate right in the ward, and are sexually disinhibited.
A 57-year-old patient, a taxi driver, always had a domineering, rude character, did not allow any initiative on the part of his wife and children, completely controlled the spending of money in the family, was jealous, and abused alcohol for many years. Over the past year, his character has changed dramatically: he became complacent and sentimental, stopped actively taking care of the car, could not figure out minor breakdowns, and left any repairs to his sons. He continued to work as a driver, but forgot how to navigate the city and was constantly asking passengers for directions. He stopped drinking alcohol and did not delve into family affairs and the family budget. I didn’t do anything at home, didn’t watch TV, because I didn’t understand the meaning of the programs. In response to the television announcer’s address “Good evening!” often answered: “Good evening to you too!” He often began to hum songs out loud, but could not remember many of the words and constantly replaced them with a meaningless “hoo-oo,” and tears always appeared in his eyes. He didn’t understand why his family brought him to the doctor, but he didn’t mind hospitalization at all. In the department he made immodest compliments to female doctors and nurses.
A computed tomography examination revealed signs of brain atrophy with predominant damage to the frontal cortex.
The cause of total dementia is direct damage to the cerebral cortex. These can be diffuse processes, for example, degenerative diseases (Alzheimer's and Pick's disease), meningoencephalitis (for example, syphilitic meningoencephalitis - progressive paralysis), dementia after self-hanging. However, sometimes a small pathological process in the area of the frontal lobes (local trauma, tumor, partial atrophy) leads to a similar clinical picture. Significant fluctuations in the condition of patients are usually not observed; in many cases, there is a steady increase in symptoms.
Thus, the division of dementia into total and lacunar is not a pathological, but a syndromic concept, since the cause of lacunar dementia is diffuse vascular processes, and total dementia can arise due to local damage to the frontal lobes.
Epileptic (concentric) dementia is essentially one of the varieties of organic dementia.
As with other organic processes, with epilepsy in the later stages of the disease, memory and the ability to conceptual activity are impaired. However, there are significant features of thinking and personal changes. The main feature of thinking is extreme rigidity, expressed by increasing thoroughness of thinking, a tendency to detail, difficulty finding words and a decrease in vocabulary (oligophasia). The lack of words is replaced by multiple repetitions, filler words and stamped (“standing”) phrases. Personal changes are characterized by exaggerated pedantry, sweetness, and a tendency to use diminutive expressions combined with despoticism and egocentrism. Narrowing the range of interests and concentrating on one’s own problems are very typical. This often leads to complete ignorance of socially significant events. Memory disorders are selective in nature: patients remember well the facts that are most important to them personally (the names of doctors, the names of medications they take, the size of the pension and the day it was issued), but they do not remember events at all that are of little importance to them. With high demands on others and a declared desire for order, patients themselves may not comply with doctors’ demands and can be rude to junior hospital staff and other patients. A decrease in the ability to generalize is expressed in the inability to distinguish the main from the secondary, in the specific situational interpretation of proverbs and sayings.
Schizophrenic dementia differs significantly from dementia due to organic disease.
In schizophrenia, memory is practically not affected, and there is no loss of the ability to think abstractly. At the same time, his harmony and focus are disrupted, and passivity and indifference increase. A characteristic symptom is fragmentation (schizophasia). Typically, patients lack the desire to achieve results. This is expressed in the fact that they, without trying to answer the doctor’s question, immediately declare: “I don’t know!” Physically strong patients with a fairly good stock of knowledge are completely unable to work, because they do not feel the slightest need for work, communication, or achieving success. Patients do not take care of themselves, do not attach importance to clothing, and stop washing and brushing their teeth. At the same time, their speech often contains unexpected highly abstract associations (symbolism, neologisms, paralogical thinking). Patients usually do not make gross errors in arithmetic operations. Only at the final stages of the disease does prolonged “inactivity of the intellect” lead to the loss of the accumulated stock of knowledge and skills. Thus, the central disorders in schizophrenic dementia should be considered impoverishment of emotions, lack of will and disruption of the harmony of thinking. More precisely, this condition should be designated as apathetic-abulic syndrome (see section 8.3.3).
BIBLIOGRAPHY
- Averbukh E.S. Mental disorders in late life. Psychiatric aspect of gerontology and geriatrics. - L: Medicine, 1969. - 284 p.
- Zeigarnik B.V. Pathopsychology. — 2nd ed. - M.: Moscow State University Publishing House, 1986. - 240 p.
- Kovalev V.V. Semiotics and diagnosis of mental illness in children and adolescents. - M.: Medicine, 1985.
- Rozinsky Yu.V. Changes in the psyche with damage to the frontal lobes of the brain. - M.: Medicine, 1948. - 147 p.
- Sternberg E.Ya. Gerontological psychiatry. - M.: Medicine, 1977. - 216 p.
- Jaspers K. General psychopathology: Trans. with him. - M.: Praktika, 1997. - 1056 p.
If you find an error, please select a piece of text and press Ctrl+Enter.
Pages: 3
Prognosis and prevention
The prognosis for apathetic dementia is influenced by such factors as the timeliness of treatment, so it is important to seek qualified help at the first manifestations of the disease. At the initial stage, the patient does not lose everyday skills and is contactable. Changes occur in his thinking, which are reflected in his speech. Gradually, the patient withdraws into himself, loses practical skills, experiences apathy and indifference to his surroundings.
With proper and timely treatment, cognitive functions can be partially or completely restored, and the person can return to normal life. Ignoring the disease leads to apathy, autism, delirium, abulia, etc. As a result, the chances of recovery are reduced to a minimum.
Prevention of the onset of dementia consists of maintaining a daily routine and stable sleep. It is important to maintain a person’s mental calm and provide him with peace. There are no restrictions on communication with other people. The exception is people, after contact with whom the patient becomes anxious and feels restless.
Thinking and memory disorders
The peculiarities of thinking disorders in schizophenic dementia are that it is not disintegration that occurs, but a distortion of thought processes (generalization, abstraction, analysis, synthesis, classification, construction of logical connections).
This is expressed in:
- mentism – a sudden “influx” of thoughts with a lack of logical connection;
- sperunge - a break in thoughts in the middle of a phrase;
- slipping - the patient begins to speak, loses the “thread of reasoning”, moves on to another topic;
- reasoning (idle talk) - lengthy meaningless reasoning
- autistic thinking - the patient’s speech is directed “inward”, meaning is attached to special attitudes and fantasies that are incomprehensible to others;
- symbolism - understanding things in a figurative pathological sense, insignificant objects are given a special meaning;
- perseverations - the patient gives the same answer to different questions;
- fragmentation - complete loss of logic in speech;
- “verbal okroshka” - incoherent, incomprehensible speech.
Memory in schizophrenic dementia lasts quite a long time.
Speech disorders
Speech disorders are represented by:
- neologisms - the inclusion into speech of new words invented by the patient;
- verbigerations - the patient endlessly repeats the same words and phrases, rhymes them;
- echolalia - the patient repeats the last syllables, words of spoken speech;
- schizophasia (speech confusion) – speech is meaningless;
- mannerism - the patient speaks in florid “abstruse” sentences, as if reading a scientific report.
Forecast. Prevention
To prevent Alzheimer's disease, there are no specific drugs that would be 100% likely to save a person from this disease.
However, many studies show the effectiveness of certain measures that can prevent or slow the progression of Alzheimer's disease.
- Physical activity (improves blood supply to the brain, reduces blood pressure, increases tissue tolerance to glucose, increases the thickness of the cerebral cortex).
- Healthy diet (especially the Mediterranean diet, rich in antioxidants, omega-3, 6 fatty acids, vitamins).
- Regular mental work (slows down the development of cognitive disorders in patients with dementia).
- Hormone replacement therapy in women. There is evidence that hormone therapy is associated with a reduced risk of dementia by a third.
- Reducing and controlling blood pressure.
- Reducing and controlling serum cholesterol levels. An increase in blood cholesterol above 6.5 mmol/l increases the risk of developing Alzheimer's disease by 2 times.
Related posts:
- Alcohol psychosis. Symptoms and treatment Alcoholic psychosis is a disorder of mental activity as a result of prolonged…
- Panic disorder and pregnancy planning A panic attack is an acute attack of anxiety and unreasonable fear,…
- Female Sexual Arousal Disorders Sexual arousal disorders were previously known as frigidity in women...
- Attention deficit hyperactivity disorder Attention deficit disorder (ADD) is a biological immaturity of the brain. How…
Types of dementia and specifics of mental symptoms
Assessing the mental status of a patient with dementia is necessary to select the correct treatment strategy.
Despite the commonality of clinical signs, with a thorough examination it is possible to identify symptoms characteristic of a particular type of dementia. Accurate diagnosis allows you to avoid errors in prescribing medications that can cause severe side effects that threaten the health and life of the patient. The most specific mental signs in the most common forms of acquired dementia
| Type of dementia | Mental symptoms |
| Alzheimer's disease | a gradual and relatively uniform increase in the rate of decline in memory, thinking, judgment, and changes in the core of personality. |
| Vascular dementia | spasmodic nature of the course, intensifying after each subsequent stroke, the presence of motor defects: paresis, paralysis. |
| Dementia with Lewy bodies and Parkinson's disease | sudden fluctuations in mental functions in the early stages from episodes of activity and critical perception to complete apathy and insanity. |
| Frontotemporal brain defects (Pick's disease) | primary damage to speech, behavior, abstract and logical thinking. |
The mental status of vascular dementia reaches its maximum levels, primarily in persons with chronic cerebral circulatory insufficiency. The high prevalence of cardiovascular pathology among elderly and senile people has led to the manifestation of cognitive dysfunction in almost every second person with acute disorders of cerebral blood flow.
Mental damage includes dementia or mental retardation, but these two types of intellectual disorders differ significantly from each other in the nature of their origin. Oligophrenia is mental retardation of congenital pathogenesis or infantile underdevelopment of the psyche, while organic dementia leads to the disintegration of knowledge and practical skills already formed in the process of life.
The speed of development of mental disorders depends on the localization of the pathological process, the quality of care, and the general physical condition of the affected person. On average, the period of degradation of brain activity takes 5-7 years. The final terminal stage of the disease dooms the patient to lifelong disability, social and everyday maladjustment.
How to make a diagnosis
To identify dementia, diagnostics are required, which includes consultations with doctors of various specialties, laboratory and instrumental tests. The diagnosis of senile dementia is often made incorrectly, since it may not be possible to confirm it (brain scans are not performed to save money).
Examination and history taking by a neurologist
At the stage of initial contact with a doctor, complaints from the patient and his relatives are collected, and the state of the patient’s nervous system is analyzed. For this purpose, neurological tests are carried out, during which a person’s motor activity, reflexes, and sensitivity are analyzed.
Such a simple study allows you to determine whether there is damage to the cerebral cortex, subcortical structures or peripheral nerves. Already during the initial examination, the doctor may suspect the presence of dementia and its cause: it appeared due to structural changes in the nervous tissue or due to age-related metabolic disorders.
To assess the patient's cognitive abilities, special tests are performed:
- 6CIT is one of the most reliable ways to identify thought process disorders;
- MIS is a test that helps identify memory impairment;
- Raven's test - identifies signs of cognitive impairment in older people;
- Beck scale - helps to determine the emotional state of the patient (one of the signs of dementia is a sharp change in mood and temperament);
- night sleep quality scale;
- simple graphic tests (ask you to draw a clock, geometric shapes, write phrases, etc.).
Consultations with doctors of related specialties
After the examination, the neurologist refers the patient to other specialists for a detailed examination. It helps to assess the general condition of the patient’s body and identify the cause of cognitive decline.
First of all, the patient should be examined by a therapist. It identifies signs of cardiovascular diseases, hypovitaminosis, and neoplasms that can provoke the appearance of signs of dementia.
To do this, it is necessary to assess the condition of the digestive tract, heart, blood vessels, kidneys and liver, since these processes affect their work. To objectively assess the functions of internal organs, it is necessary to conduct laboratory tests and instrumental tests.
Laboratory and instrumental diagnostics
Analyzes and instrumental studies are the final stage of diagnosis, the results of which confirm or refute the preliminary diagnosis.
Necessary studies for diagnosis of dementia and differential diagnosis
| Type of study | Pathologies that it helps to identify |
| General blood analysis | Anemia, inflammatory processes, blood diseases (leukemia) |
| Blood chemistry | Impaired kidney and liver function, digestive problems |
| Ultrasound of the abdominal organs | Structural changes in the liver, kidneys, pancreas |
| Angiography of cerebral vessels | Pathologies of the vascular bed that lead to impaired blood circulation and metabolism in the central nervous system (atherosclerosis, strokes, hypertension, etc.) |
| CT or MRI of the brain | Brain neoplasms, signs of degeneration of the cortex or subcortical structures |
Based on these research methods, the doctor makes a diagnosis of dementia or rejects it. If dementia is caused by another disease (hypertension, atherosclerosis, neoplasms, Alzheimer's or Parkinson's disease), then treatment of the primary pathology is carried out. With successful therapy, symptoms of dementia decrease or disappear altogether.
The diagnosis of vascular dementia is established in the presence of circulatory disorders in the brain. This occurs due to deterioration of vascular patency by blood clots, atherosclerotic plaques, or compression by tumors.
If the examination does not reveal a pathology that can lead to a decrease in mental abilities, then a diagnosis of senile or idiopathic (the cause is unknown) dementia is established. Then the treatment is aimed at supporting blood circulation and metabolic processes in the tissues of the central nervous system. Such treatment cannot completely eliminate the disease; it only reduces the rate of development of changes and improves the patient’s quality of life.
Features of dementia treatment
Treatment of dementia depends on the cause of the disease; individual and complex therapy is used. The main methods of treatment in the first stages are reduced to the use of general strengthening agents and nootropic drugs.
Commonly accepted treatments for dementia:
- drugs that ensure normal blood circulation in the brain;
- taking antipsychotics;
- adding foods containing antioxidants to the diet;
- regular monitoring of blood pressure.
For vascular dementia, treatment is carried out using other methods. Therapy is aimed at the main source of neuronal death. These are high blood pressure, vasculitis, atherosclerosis. In addition to medicinal use, you should normalize your diet and stop smoking. It is important to practice simple physical and mental exercises. Doctors note that old age is not a reason to give up some physical activity. Daily walks are recommended for the prevention and treatment of dementia. Regular hiking protects brain cells from destruction.
Other types of disease and their brief characteristics
In medicine, there are types of dementia that are not so widespread. According to the ICD, this type of disease is designated by code F02.8.
- Progesterone dementia is a pathology that develops during pregnancy under the influence of hormone imbalance. During pregnancy, progesterone increases, which affects the nervous system. Disorders are aggravated by stress. The main signs in a woman: forgetfulness, anxiety, constant fatigue. Then difficulties arise in formulating thoughts, spatial orientation, depression gives way to euphoria.
- Vascular dementia. Variant of vascular dementia. Develops as a result of vasculitis (autoimmune inflammatory vascular disease). The symptoms are identical to those of the vascular type.
- Concentric dementia. It most often affects children and adolescents suffering from long-term, severe forms of epilepsy. All mental processes in the patient slow down: memory, thinking, perception. This makes the child's further education impossible.
- Parlor dementia is a mental disorder that manifests itself in the lack of one’s own judgment and the desire to learn something new. The patient compensates for the deficiency with memorized phrases and refined manners.
- Frontotemporal dementia is an inherited disease that affects the frontotemporal lobes of the brain. Brain neurons are lost, many atypical cells appear. The cause is considered to be an intrauterine chromosomal abnormality.
- Post-stroke marasmus . Post-stroke dementia develops after a stroke. When a hemorrhage occurs in the brain, some parts of it die. In addition to impaired memory and thinking, the patient's sensitivity is impaired, motor functions are partially lost, and urinary incontinence occurs.
- Intellectual dementia is an acquired intellectual disorder. Characterized by loss of cognitive functions: thinking, attention, memory. It becomes impossible to use previously acquired skills. The patient's character changes, his personality degrades.
- Dementia of complex genesis is moderately severe . The cause of the pathology is a complex of diseases. Different parts of the brain are affected, which contributes to the appearance of various symptoms. Personality changes are not pronounced, the patient retains the ability to care for himself.
The disease should be treated, since at the second stage the changes will be irreversible and will lead to complete degradation of the personality.
Each type of senile insanity is characterized by its own cognitive impairment. Only in some cases is there a combination of multiple symptoms. The doctor’s task is to determine the source of progressive dementia.
Therapy is prescribed in accordance with the disease that triggered the process of brain cell degradation . The classification of the disease is adopted to identify the root cause of the pathology and prescribe adequate treatment.
Dementia and psychology
Dementia in psychology is an almost irreversible, persistent decline in the level of mental activity, accompanied by mental disorders. A psychologist diagnoses the patient’s mental state as a whole, analyzing emotional, cognitive, motivational and volitional processes and finally formulating a pathopsychological diagnosis.
The clinical and psychological structure of dementia can be divided into negative and positive. Negative symptoms include loss of mental functions, mental defects, and personality disintegration. Negative symptoms are stable and resistant to therapy by a psychologist.
Positive symptoms are more dynamic, may become more complex, but are partially reversible. It includes obsession, mania, hallucinations, delusions and other pathological formations of the psyche that appear throughout the illness. Often with dementia, a psychologist identifies one of the pathopsychological syndromes as the leading one.
The psychological and pedagogical characteristics of dementia relate mainly to dementia in childhood, an important sign of which is the loss of already acquired knowledge. It is characterized by secondary, uneven cognitive deficits, a patchwork of impairments, and a clear discrepancy between changes in personality and the stock of knowledge. In the practice of a psychologist, we often encounter a decrease in self-criticism, motivational weakness, and loss of higher emotional manifestations.
A psychologist not only diagnoses mental changes, but also deals with issues of psychosomatics. The psychosomatics of dementia is manifested by exacerbation and worsening of the underlying disease due to traumatic experiences, a change of environment, and relatives’ rejection of dementia as a disease. Since the mental life of a dementia patient is reduced to a monotonous and primitive course, frequent behavioral disorders, the psychologist is called upon to help loved ones understand the situation and learn the rules of behavior with such a person. This allows you to reduce the frequency of exacerbations, slow down the progression of dementia, improve its course, remove antipsychotics from the treatment structure and make life easier for both the patient and caregivers.
The first symptoms of the onset of dementia
What time dementia begins depends on many factors, not just old age. In some diseases and circumstances, dementia can develop at a very early age, even in adolescence.
People at risk are those who:
- have a hereditary neurodegenerative or genetic disease (Parkinson's, Pick's, Huntington's, Down's syndrome);
- have disturbances in the functioning of the endocrine system;
- suffered serious poisoning (from drugs or chemicals) or worked in hazardous industries or agriculture (with frequent contact with chemicals);
- have diseases associated with the blood vessels of the brain;
- suffered oxygen deprivation, stroke;
- suffered from neurosyphilis, panecephalitis, meningoencephalitis;
- infected with AIDS;
- have brain tumors;
- suffer from diabetes;
- have close relatives with a confirmed diagnosis of dementia;
- suffer from alcoholism;
- received a traumatic brain injury.
The presence of at least one of the factors significantly increases the risk that sooner or later signs of dementia will appear.
What to look for Symptoms of the onset of dementia Emotional state A person at the initial stage becomes apathetic, loses interest in hobbies, loved ones and acquaintances. Becomes secretive and uncommunicative If there are no objective reasons for such behavior, then such an emotional state may indicate the onset of dementia. With the further development of the disease, his mood often and unexpectedly changes: from apathy to excitement, euphoria or aggression. Such emotional “swings” should immediately alert relatives. Speech One of the very first signs of the onset of the disease is changes in speech. Neurons decay in the brain, memory gradually deteriorates, which is reflected in the patient’s speech from the very beginning. It is difficult for him to construct sentences and select the words that are necessary for their meaning. Because of this, speech becomes slow, sentences are shorter (over time they are reduced to individual words). With some types of dementia, the patient may completely refuse to talk, and so-called “imaginary muteness” occurs. Fine motor skills This sign of the onset of dementia is not so clear and is characteristic of certain forms of the disease. However, it should not be overlooked. In the frontotemporal form, it is the lack of coordination of movements and hand tremors that appear earlier than changes in speech. Difficulty performing tasks that require precise movements may indicate the onset of illness. Changes in character This symptom is the most difficult to notice. The patient's character does not change suddenly, but gradually. In this case, most often there is a deterioration of certain character traits
If a person was frugal, then with the onset of the disease he may become stingy; caution develops into paranoia. Such signs of the onset of dementia can only be noticed with careful and frequent communication
Also, the onset of this disease is characterized by touchiness, suspicion, and tearfulness. Appearance At the onset of dementia, the critical attitude towards oneself weakens, coupled with apathy, this leads to a sloppy appearance. A usually neat and clean person begins to neglect personal hygiene and wears torn or dirty clothes. Sloppiness is reflected not only in appearance, but also in his home
Oddities in behavior are also an ambiguous symptom of the onset of dementia. To notice changes, you need to know the person well and communicate with him regularly. In most forms of dementia, short-term memory is primarily affected from the outset. That is, a person may forget a conversation that just happened and cannot remember recent events.
Due to brain atrophy, the ability to navigate in time and space and plan one’s affairs is impaired. Thinking in dementia is inhibited from the very beginning, which also becomes noticeable when communicating
These are the main signs of the onset of dementia. Depending on which area of the brain is affected by dementia, the first symptoms may be supplemented and vary slightly. In fact, the slightest changes in the behavior of a loved one should cause alarm.
Even if the diagnosis is not confirmed, such attention will not be superfluous
Types of dementia
In addition to the division into congenital dementia and acquired dementia, partial dementia is also observed, divided into the following types:
- Epileptic
, the trigger for the development of which is epilepsy. - Vascular dementia
. Atherosclerosis of the brain plays a huge role in its development. - Traumatic
, which is provoked by injuries. - Alcoholic
. Brain damage occurs due to alcohol abuse. - Schizophrenic
. She is accompanied by schizophrenia. - Psychogenic
. It is also called imaginary dementia, which goes away on its own. - Decreased mental level
. In this case, mental activity is weakened only slightly.
Senile dementia
The reasons why dementia develops have not been fully determined. With age, all biochemical reactions in the human body slow down, some fail due to the development of illnesses. Dementia in older people begins to progress gradually. Previously acquired skills are forgotten, and a person is unable to learn new ones, just as he is unable to generalize information, draw conclusions and adequately evaluate himself and others.
Negative character traits come to the fore - stinginess, irritability, anger, envy. Interests narrow and views become stereotyped. Shame and commitment to moral and ethical standards disappear. In severe cases, complete degradation and maladjustment of the personality is observed. The patient requires constant care and supervision, because he is not able to care for himself.
Epileptic dementia
Numerous convulsive seizures lead to brain trauma and the development of this form of intellectual disorder. The main symptom is a slowdown in the pace of mental processes. A weak-minded person is not able to separate the essential from the secondary. His speech is full of cliches, but he can speak quickly and not lose track of his sentences.
In ordinary conversation, such patients have a tendency to detail everything and over-describe. At the same time, their tendency to generalize and distract suffers. Relatives have a hard time with such wards, because they “love” to teach and instruct, taking on the role of a narrow moralist. They overestimate their own life experiences, and their statements are shallow, superficial and banal.
Schizophrenic dementia
It is called transient, transient, because it occurs episodically. Patients may suddenly demonstrate good memory and thinking, but then a period of psychosis begins again. The diagnosis of dementia is made after observation and testing of reactions to various activities and tasks. With this form of illness, a person thinks abstractly, he is prone to philosophizing, far from reality. Dementia leads to a slow decline in knowledge and loss of vital skills. Problems with concentration also arise.
Against the background of intellectual impairment, the desire to communicate disappears. The patient gradually becomes autistic. In severe cases, motor ability is preserved, but the person spends almost all the time immobile. He does not control the process of eating, physiological needs and does not answer questions. The prognosis for treatment is questionable.
Alcoholic dementia
Alcohol-based drinks cause irreversible changes in the body, integrating into biochemical processes. As a result of prolonged and systematic alcohol abuse, addiction and mental disorders are formed, which result in alcoholic dementia. Intellectual disorder syndromes are observed at stage 3 of alcohol dependence. All vital functions of the intellect are damaged or completely lost. The person becomes unable to perceive information and reason. Speech and memory suffer.
Signs of dementia
There are ten typical signs of dementia.
The first and earliest sign of the development of dementia is considered to be changes in memory, and above all, short-term memory. The initial transformations are almost invisible. For example, a patient may remember events from his past youth, but not remember the foods he ate for breakfast.
The next early sign of developing dementia is speech disorders. It is difficult for patients to find the right words; it is difficult for them to explain basic things. They may try in vain to find the right words. A conversation with a sick person suffering from the early stages of dementia becomes difficult and takes more time than it previously did.
The third sign can be considered changes in mood. For example, depressive moods are constant companions of early dementia.
Apathy and lethargy can be considered the fourth sign of the pathology in question. A person suffering from dementia loses interest in previously enjoyed activities or their own hobbies.
The fifth sign is the appearance of difficulties in performing ordinary tasks. For example, a person is unable to check his credit card balance.
Often in the early stages of dementia, a person feels confused. Due to a decrease in memory function, mental activity and judgment, confusion arises, which is the sixth sign of the described disorder. The patient forgets faces, adequate interaction with society is disrupted.
The seventh sign is difficulty remembering plot lines, difficulty reproducing a television program or conversation.
Spatial disorientation is considered the eighth sign of dementia. Sense of direction and spatial orientation are common mental functions that are among the first to be impaired in dementia. The patient ceases to recognize familiar landmarks or is unable to remember previously constantly used directions. Moreover, it becomes quite difficult for them to follow step-by-step instructions.
Repetition is a common sign of dementia. People with dementia may repeat daily tasks or obsessively collect unwanted items. They often repeat questions that have already been answered before.
The last sign can be considered disadaptation to change. People suffering from the described illness are characterized by a fear of change. Because they forget familiar faces, are unable to follow the speaker’s thoughts, forget why they came to the store, they strive for a routine existence and are afraid to try new things.