Stupefaction is a person’s disorientation in space and time, which can be accompanied by a violation of self-identification, as well as delusions and hallucinations.
There may be a short-term, transient state of confusion that is not associated with medical problems. For example, while falling asleep, after a sudden awakening, especially during dreams, etc. After a few seconds, or at most minutes, consciousness is completely restored. However, if such a condition lasts for several hours, days or even weeks, and is aggravated by increasingly greater manifestations of disorientation, we are talking about diseases or disruption of brain activity.
Twilight stupefaction - what is it and how does it manifest?
A twilight state of consciousness is a mental state with deep disorientation, limitation of consciousness on certain objects or persons, accompanied by psychomotor restlessness and aggression.
An episode of twilight disorder of consciousness is subsequently replaced by complete amnesia; the person cannot remember how he behaved, what happened around him during the narrowing of consciousness.
In clinical practice, there are often cases when a person unknowingly leaves for another city or region. He subsequently describes his state as follows: “Sitting on the bus, I seemed to think or close my eyes for a few seconds... I didn’t understand how I ended up in a place unfamiliar to me. I asked a passerby, it turned out I was in another city...” However, not in all cases this violation is harmless; a person can unknowingly seriously injure or kill, and with frantic cruelty.
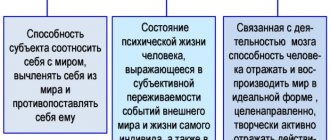
Twilight disorder of consciousness refers to disorders of higher mental processes. With the help of consciousness, a person learns about the world around him, himself, and adapts to changing environmental conditions.
Being in a clear consciousness, a person easily relates himself and the surrounding reality, soberly assesses his capabilities. In this case, they say that he is correctly oriented in location, time, surrounding situation and his own personality.
Oneiroid
Oneiroid is a more severe form of clouding of consciousness. In this case, the defining feature is a dream-like delirium of fantastic content, which unfolds dramatically and leads to a violation of the patient’s level of self-awareness. Visions are perceived as if by the inner eye; they absorb almost all of a person’s attention and draw him into the illusory world. The scenes are large-scale, fantastic, colorful and dynamic. The patient feels like a different person or being, with unusual capabilities and the ability to influence everything that happens. It is as if he controls world wars, discovers new galaxies, collects plants of extraordinary beauty, meets historical figures or even becomes them.
Unlike the oneiroid, all these vivid experiences have practically no effect on the behavior of the person in the oneiroid. He may appear distracted, lethargic, or simply freeze periodically. His movements are usually elaborate, meager, and slow. From them and from their frozen facial expressions it is almost impossible to guess the content of the visions. At the same time, it is sometimes possible to obtain simple answers to questions about the patient’s experiences and imaginary place of stay.
Such clouding of consciousness can occur in stages:
- Another controlled fantasy with an influx of images;
- Delirium of intermetamorphosis with a feeling of unreality and staging of events, false recognitions, developing into sensual delirium of fantastic content;
- Oriented oneiroid, when dream-like experiences are combined with partial orientation in the environment;
- A deep oneiroid with detachment from the real world; when leaving it, there is complete amnesia of the actual events that have occurred.
Sometimes oneiric stupefaction is diagnosed after its completion. At the same time, the patient has a detailed, vivid description of fantastic experiences combined with a paucity of memories of what is happening around him and bewilderment about the dissonance regarding the duration of the episode and his own personal identity.
Main features
4 main signs of impaired consciousness:
- detachment from reality: a person does not understand what is happening around him, attention is narrowed to one or several objects, he is not interested in people and external circumstances,
- allo- and autopsychic disorientation of varying degrees of severity: impaired perception of place, time, one’s personality,
- thinking disorder: a person is unable to clearly express his thoughts and answer questions asked, speech is confused, incoherent,
- memory impairment: after the state is normalized, a fragment during which consciousness was narrowed falls out of memory.
Twilight disorder of consciousness is associated not only with disorientation, but also with various automatisms - stereotypical, sharp, repetitive movements, sometimes even of a professional nature: during a twilight disorder, a carpenter makes movements as if working on a machine, an operator continues to work on an assembly line, and a bus conductor – sell tickets to imaginary passengers.
As a rule, most often a person is in motor agitation, moves chaotically, movements are not purposeful and destructive in nature.
There are several types of mental automatisms: trance and fugue. During trance, ambulatory automatisms have a complex structure; movements from the outside seem quite consistent. However, these actions were not planned by the person himself; they are ineffective.
Most often, patients with this variant of twilight narrowing of consciousness are prone to moving, traveling in transport, and unknowingly leaving for another city or region. Outwardly, one notices a drowsy appearance and a certain confused detachment from what is happening. The trance can last from several minutes to several days.
A fugue is a sudden change of state with the need to escape or run. Movements are also aimless and unrelated to the environment. The fugue is short-lived, only a few minutes.
A narrowing of consciousness occurs suddenly against the background of emotional stress, anger, rage, fear. Both hallucinatory and illusory experiences at the height of affect are characteristic.
Twilight disorder can occur not only during the day. Disturbances that occur at night are called somnambulism or sleepwalking.
What Causes Brain Fog?
This condition sometimes occurs in healthy people as a result of fear, shock, prolonged standing, or staying in one position. But with a cloudy head, the causes can also be represented by more serious diseases. If such problems occur frequently (more than once a month), consult a doctor.
Causes of brain fog in healthy people:
- Prolonged standing, which can also cause cramps. These symptoms may also indicate chronic venous insufficiency.
- Rapid changes in body position, for example when standing up from a sitting position. We are talking about orthostatic hypotension, which is a drop in blood pressure with a rapid change in posture. This condition can be supported by certain medications.
- Prolonged tilting of the head (for example, when looking at the sky), causing a decrease in blood flow to the head.
- Prolonged stay in a room with “heavy” air.
- Fright.
- Emotional excitement, nervousness.
- Swallowing.
- Defecation.
- Urination.
- Shaving or tying a tie.
- Phobias, looking at unpleasant things (blood, needles, arachnophobia, fear of heights, other phobias).
- Emotional trauma.
- Depression.
- Exhaustion.
- Dehydration.
- Intoxication.
- Sudden or severe pain.
- Severe cough, sneezing.
- Laughter.
- Poor or insufficient sleep.
- Playing sports in high ambient temperatures.
- Hormonal changes.
- Pregnancy (increased cardiac output).
For brain fog, causes may include medications. These include medications for hypertension, allergies, depression, and nausea.
Tablets that may make your head feel cloudy:
- opioid analgesics (at the beginning of use, as a rule, symptoms decrease over time);
- parasympathomimetics (by lowering blood pressure);
- sympatholytics used to reduce blood pressure, tachycardia (blocking norepinephrine receptors);
- antidepressants;
- combinations of antidepressants or their use with opioids - can lead to thought disorders, serotonin syndrome (CNS irritation, tremor, muscle twitching, impaired consciousness, hypertension, rapid heartbeat);
- diuretics.
Brain fog as a symptom of illness
People with a number of diseases, such as diabetes, heart disease, atherosclerosis, chronic lung diseases, and people prone to panic attacks are more prone to feeling brain fog.
However, this condition may be one of the symptoms of other pathologies:
- cardiac arrhythmias, heart rhythm disturbances due to pulmonary embolism, obstruction in the pulmonary bed - with these disorders the brain does not receive a sufficient amount of oxygenated blood;
- heart tumors that cause obstruction of blood flow, manifested, in particular, by fatigue, heaviness in the body, and inability to perform normal physical activities;
- hypertrophic cardiomyopathy - a condition in which the heart wall is normal, but the capacity of the heart is insufficient; because of this, it does not receive enough blood and works ineffectively;
- aortic stenosis or narrowing of the aorta - like heart tumors, these conditions cause insufficient blood supply to the brain and are characterized by drowsiness, inability to concentrate, and inability to perform normal physical activities;
- chronic venous insufficiency – prevents blood from returning to the heart;
- cerebrovascular disease, cerebral vascular disorders, such as narrowing of the arteries that supply blood to the brain;
- migraine;
- vegetative-vascular dystonia (VSD);
- some mental illnesses, neuroses;
- acute myocardial infarction;
- cervical osteochondrosis with compression of blood vessels or nerves;
- cold, ARVI.
How does a disorder of consciousness occur?
Consciousness is disrupted sharply and suddenly, without any prerequisites. The condition returns to normal just as quickly, leaving no consequences on the person’s well-being.
With the dysphoric version of twilight disorder of consciousness, the patient looks detached from the world around him, his facial expression is angry, anxious. Productive contact with a person in this state is impossible. The behavior does not correspond to what is happening. Criticism is completely lost.
With hallucinatory twilight disturbance of consciousness, bright, imaginative, threatening hallucinations occur. More often, these may be auditory or visual hallucinatory phenomena that cause aggressive or defensive behavior in a person.
Destructive behavior can be directed at objects or even people. Stereotypical actions are carried out with particular force and cruelty, for example, while in a twilight state of consciousness, a person can inflict 30 or more stab wounds.
In delusional twilight disorder, behavior is determined by a delusional interpretation of what is happening. More often, delusions of persecution occur; the patient either takes a defensive position or seeks to escape from imaginary ill-wishers.
Medical classification
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Disorientation is classified into radiation, occupational, spatial and social symptoms. Psychiatry identifies the term “autopsychic disorientation” - the lack of perception of personal factors (the inability to reproduce the last name, first name, patronymic, date of birth, that is, identification data). With this phenomenon, the individual’s surrounding world changes, and orientation in it is completely absent. A double perception of the world is noted, a real and imaginary environment is created, alternately visited by the psychological inner world. The full picture emerges after a proper examination by a doctor.
What diseases can it occur in?
Twilight syndrome can occur in various mental illnesses and pose a significant danger to society.
Twilight states can be functional (affective, hysterical, psychogenic) and organic (epileptic or epileptiform syndrome).
Twilight syndrome is observed in hysterical psychoses. The occurrence in this case is associated with a traumatic situation. Consciousness narrows at the height of significant experiences and violent emotional reactions. In behavior one can note theatricality, infantilism, pseudo-dementia. It is possible to distinguish from twilight states of organic origin by EEG: changes in hysterical psychoses are not detected.
With schizophrenia, delusional disorientation may occur: at the height of delusional experiences, a person can be completely cut off from the outside world, immersed in his own painful reality. You lose orientation in time, place, and sometimes even in your own personality. After emerging from the twilight disturbance of consciousness, islands of recollection may remain in the memory, which are subsequently interpreted deliriously, and residual delusion arises.
In case of amnestic disorientation, which occurs in severe head injuries and dementia, the narrowing of consciousness is associated with severe memory impairment.
In a severe depressive state against the background of decreased mood, volitional and critical components, apathetic disorientation with detachment from the outside world may occur.
Most often, twilight disorder of consciousness occurs with epilepsy and may follow a seizure or be its equivalent. Sometimes an attack of impaired consciousness is preceded by a so-called aura, when the patient feels the approach of an attack, is bothered by a headache, photophobia, increased sense of smell, etc. A person may notice sleep disturbances, sudden mood swings towards angry-angry and dysphoric affect.
There is an oneiric variant of twilight disorder of consciousness. It is characterized by an abundance of vivid, fantastic hallucinations and catatonic manifestations.
There are twilight episodic disturbances of consciousness: simple twilight, impulsive, hallucinatory, expansive, psychomotor. The clinical picture reveals a period of precursors with insomnia, asthenia, and fatigue. After the twilight contraction in this case, a long, deep sleep occurs.
Possible complications
Psychiatrists divide the negative consequences of the disorder into two groups: those associated with the primary disease and those associated with inappropriate human behavior. Twilight stupefaction can occur against the background of organic pathology, and therefore characteristic complications may include:
- With epilepsy, personality disorders develop - isolation, indifference to others. Gradually, apathy towards work and hobbies appears. This is due to organic changes in the nerve centers in the cerebral cortex, as well as side effects of long-term use of antiepileptic drugs.
- With the growth of intracerebral tumors, the neurological deficit gradually increases. Sensory disturbances, movement disorders, blurred vision, etc. may occur. With rapid growth of the tumor, there is a risk of displacement of brain structures with their pinching in the foramen magnum, which can be fatal.
The main consequence of impaired consciousness is the patient’s antisocial behavior. Due to the development of hallucinations or delusions of persecution, he poses a threat to others and himself. Attempts at suicide, aggression towards loved ones, colleagues or strangers are possible. In some cases, patients commit brutal murders without remembering anything about what they did.
Diagnostics
The diagnosis of twilight disorder of consciousness is made on the basis of clinical data and the patient’s behavior. Certain difficulties in forensic psychiatric examination are presented by the diagnosis of oriented twilight disorders, in which traces of orientation are preserved (recognition of loved ones, particles of self-awareness), and there are no delusions and hallucinations.
Patients give the impression of people who are not completely awake (unsteady, shaky gait, slurred speech).
In case of twilight syndrome of organic origin, a more complete examination is necessary: MRI of the brain, EEG, consultation with a neurologist. When diagnosing epilepsy - consultation with an epileptologist and EEG with stress tests and dynamics.
Stun
Stunning is a pathology that has a distinctive feature - mental impoverishment. The patient's behavior becomes more withdrawn, with slow coordination of movements, detached, in a state of prostration. He does not clearly understand the speech in the dialogue and answers inaccurately. But this stage of the disease does not have obvious mental disorders. The person does not experience aggression, there are no hallucinations, high levels of confusion, or insomnia. If left untreated, this stage can become more complex, causing the person to stop speaking, then stop moving and become comatose. The initial stage of stunning is called nullification.
Are disorders of consciousness treatable?
Dysphoric, hallucinatory and delusional variants of twilight disorder of consciousness pose a public danger. A person can commit crimes with extreme cruelty.
First aid for narrowing of consciousness is to isolate the patient to exclude the possibility of self-harm or harm to others until the ambulance arrives. If possible, the limbs should be immobilized, and diazepam should be administered to relieve psychomotor agitation.
The patient is hospitalized in a psychiatric ward, where therapy with tranquilizers and antipsychotics continues until the pathological condition emerges. The cause of the narrowing of consciousness is being clarified. If this is a pathology of organic origin, the underlying disease is treated under the supervision of a neurologist.
Reasons for the development of the syndrome
Amentia syndrome occurs due to severe physical or mental exhaustion based on poisoning with an endogenous or exogenous toxin. The cause of a mild form of amentia can be:
- diarrhea;
- mild poisoning;
- blood loss;
- prolonged surgical intervention.
A severe form of the disease occurs when:
- open or closed craniocerebral injury;
- organic brain damage;
- hyperthyroidism;
- infectious disease;
- acute and chronic intoxication due to alcohol consumption and drug addiction.
The most profound manifestations of the disease are observed in sepsis, which is accompanied by brain damage. Bipolar affective disorder and some forms of schizophrenia can cause short periods of amenity.
This pathological condition can last a long time. During this, a person loses all types of orientation.
With amentia, the baggage of a lifetime’s experience is lost, skills and abilities are lost, new information is not stored in the brain and is not remembered.