Epilepsy is a chronic disease in the human brain, the manifestation of which is directly related to the occurrence of recurrent epileptic seizures, accompanied by various clinical manifestations and specific symptoms. Among the complementary clinical manifestations of the pathology, doctors name characteristic changes in the psyche, and among the specific symptoms, changes of a specific nature related to the bioelectrical activity of the brain, detected during electroencephalography, stand out.
The progress of the pathology is associated with the development of the epileptic focus. An epileptic focus is a group of nerve cells that have increased excitability and the ability to generate sudden excessive neuronal discharges. Such discharges can spread to part of the brain or the entire brain from the focal zone and cause an epileptic seizure, which is characterized by transient functional disorders in the brain.
Classification of attacks (convulsions)
Generalized seizures
Content:
- Classification of attacks (convulsions)
- Causes
- Symptoms of the disease and manifestations of attacks
- Stages of the disease
- Diagnosis of the disease
- Treatment methods
- Limitations and recommendations
- Nutrition for illness
- Living with epilepsy
- How dangerous is the disease?
- Assignment of disability
Convulsions with synchronized discharges in both hemispheres of the brain are generalized. When they occur at the onset of seizures, the entire cerebral cortex is immediately involved in the process. You can usually verify the occurrence of such attacks by performing electroencephalography. In the case of generalized seizures, patients do not have warning signs (auras), and people lose consciousness immediately when the attack begins.
Generalized seizures have several types. The most common generalized epileptic seizures found in medical practice are tonic-clonic, clonic, atonic, tonic, myoclonic and absence seizures.
Tonic-clonic and clonic
The traditional name for tonic-clonic seizures is grand mal seizure or and mal. Such convulsions are usually accompanied by an aura, unconsciousness, and a fall in the process. The tonic stage lasts up to 20 seconds, then it is followed by the clonic stage, which lasts a little longer. With clonic convulsions, the patient experiences simultaneous twitching of the muscle fibers of the trunk and all extremities. After the end of these two stages, a post-convulsive period begins, which usually lasts several hours.
Tonic-clonic epileptic seizures can be characterized by a genetic nature; peak-wave complexes are visible on electroencephalography. Most often, such cramps bother patients in the morning immediately after waking up. It happens that such convulsions are preceded by myoclonic twitches.
If the disease is acquired, then generalized seizures are perceived as secondary on the basis of primary partial seizures. However, their cause may be brain damage - trauma, stroke, infection, tumor.
Another cause of tonic-clonic epileptic seizures may lie in drug addiction or alcoholism and their withdrawal syndromes. Metabolic disorders such as hyponatremia, hypocalcemia, uremia, and liver failure may predispose to this pathology.
Tonic-clonic seizures can occur at any age. Most often, the first time generalized convulsions occur in children under 2 years of age, and the pathology develops until the age of twenty. Or the manifestation and development of the disease begins after 60 years.
Tonic and atonic
Tonic and atonic seizures of epilepsy are very rare types of generalized seizures, accounting for only 1% of all possible ones in the human population. Most often they occur in some severe epileptic forms, the development of which occurs in early childhood, for example, in Lennox-Gastaut syndrome, myoclonic-astatic epilepsy.
Atonic seizures are sometimes called drop attacks or akinetic seizures. With them, postural muscle tone is suddenly lost, which leads to the patient falling to the ground or floor. Convulsions are not observed during such attacks. The attacks themselves end very quickly, and there are no post-ictal symptoms.
During tonic attacks, the tone of the body muscles suddenly increases, causing the patient to fall backward. Both of these attacks can cause severe damage to the brain.
In childhood, akinetic epilepsy can be expressed by hypertensive seizures, which look like extension, flexion, rotation of the limbs, torso, and head.
Myoclonic seizures
Myoclonic seizures are defined as involuntary brief flexor contractions involving part and the entire body (arms, head). Myoclonic seizures can cause patients to fall, which immediately stops the seizure. Sometimes myoclonus is not related to epilepsy. Non-epileptic myoclonus can occur as a consequence of various neurological pathologies - with damage to the spinal cord or spinal trunk.
More often than others, myoclonus is accompanied by conditions such as cerebral ischemia, acute cerebral hypoxia, Creutzfeldt-Jakob disease, and other degenerative brain processes. Also, myoclonic seizures occur in healthy people as night shudders, which is a completely normal physiological process.
Absence seizures in epilepsy
Also among generalized epileptic seizures there is also a non-convulsive type. Such attacks are called absence seizures. Absence seizures are short-lived, lasting only 3-5 seconds, and are more common in childhood. With absence seizures, consciousness turns off and the patient freezes in the position of the movement that was interrupted. The man’s face takes on a frozen form, meaninglessness is visible in his gaze, he rushes to one point. Less common symptoms include pallor or hyperemia of the face, sunken eyeballs, and tilted head. When consciousness returns, the patient can calmly continue the interrupted action. Usually, people around may not notice absence seizures and perceive them as absent-mindedness, high distractibility in children.
Absence seizures are typical and atypical. Typical ones were previously called the term “petit mal”; their peculiarity is that they belong exclusively to children. The maximum when typical absence seizures can begin is adolescence. They are characterized by their occurrence in generalized epilepsies such as childhood or juvenile absence epilepsy. Absence seizures are associated with an electroencephalographic pattern - generalized peak-wave three-hertz discharges, which can be provoked by hyperventilation, which is an excellent diagnostic technique for this condition.
With atypical absence seizures, the onset is less sudden and the disturbance in muscle tone is more pronounced. With it, electroencephalography shows slow and irregular peak-wave two-hertz activity of a generalized form, but more often asymmetrical. Atypical absence seizures occur most often in severe epileptic forms - Lennox-Gastaut syndrome.
Partial (focal) seizures
If the discharge of an epileptic seizure originates in a localized area of the cerebral cortex, then it is called a partial or focal seizure. In this case, the focus of epileptic activity is single or several, and later this activity can spread to other areas of the cortex. When activity spreads throughout the entire area of the cerebral cortex, the attack is considered to be secondary generalized.
Simple seizures
In simple partial seizures, consciousness is fully preserved, and the epileptic discharge does not go beyond the localization site. When conducting electroencephalography during an attack, one can note the localization of the epileptic discharge, which begins in a certain area of the cerebral cortex. The clinical picture of the attack will depend on the area where the discharge is localized. In one patient, simple partial seizures usually always occur in the same form.
As an example of the clinical symptoms of simple partial seizures, we can name local involuntary movement disorders (clonic or tonic convulsions), autonomic disorders, mental or sensory disorders. However, simple partial seizures can develop into complex or secondary generalized seizures.
Complex seizures
Complex partial seizures are characterized by symptoms of simple partial seizures with obligatory loss of consciousness. Such phenomena are also called psychomotor seizures in medicine. Most often they begin in the frontal or temporal lobes, and the onset can be of two types. With the first type, attacks of a complex nature begin as simple and progress, while with the second, they immediately begin with loss of consciousness.
With complex partial seizures, automatic or altered behavior of the patient often occurs: he begins to twirl objects in his hands, fiddle with his clothes, wander aimlessly, and perform strange movements or actions. Also in various combinations one can observe smacking, chewing movements, undressing, and grimacing.
In complex partial seizures, confusion always occurs in the postictal period. Also, such convulsions can develop to the state of a secondary generalized attack.
Symptomatic form
This type of pathology is of a secondary nature. The reasons for the appearance may be:
- head injuries;
- brain tumors;
- poisoning;
- neuroinfections;
- consumption of alcohol, drugs;
- dehydration;
- hypothermia or overheating;
- stroke;
- emotional stress.
As a result of exposure to unfavorable factors, partial destruction of brain neurons occurs.
Seizures may appear immediately or after some time. EEG and MRI detect organic brain lesions.
Symptoms depend on the location of the lesion and the degree of death of brain structures. The patient has:
- generalized seizures with loss of consciousness;
- seizures with or without partial loss of consciousness.
The disease may also be accompanied by mental disorders (depression, hallucinations, memory impairment, attention, paranoia), and other symptoms (headaches, dizziness, spatial orientation disorders).
Treatment is aimed primarily at eliminating the cause of the disease.
An operation is performed to remove the tumor, drugs are prescribed for detoxification and resorption of intracranial hematomas. Often the attacks stop when the provoking factors are removed.
However, if cells die irreversibly due to infection or injury, the disease cannot be cured. Then the patient is prescribed antiepileptic drugs, and the issue of disability is resolved.
Read about other types of the disease:
- epilepsy of Jackson and Kozhevnikov;
- about absence and cryptogenic;
- about generalized and partial forms;
- about myoclonic and temporal;
- about pharmacoresistant, focal and alcoholic.
Causes
In modern medicine, there is confidence that epilepsy is a consequence of a simultaneous, abnormal, strong excitation of neurons in a separate area of the cerebral cortex - the epileptogenic focus. These processes are provoked by imbalances in the balance between inhibition and excitation in the areas where the focus is localized. Neurons begin converting the excitation perceived by the human senses into electrical impulses. For the body, these impulses can be compared in strength to lightning during a thunderstorm in nature.
The causes of epileptogenic foci are:
- cerebrovascular accidents (stroke, for example);
- physical head injuries and concussions;
- chronic pathologies of the nervous system (for example, multiple sclerosis);
- infections affecting the meninges (meningitis and others);
- drug addiction, alcoholism;
- pathological development of the fetus in utero;
- hereditary factors;
- tumors in the brain;
- metabolic dysfunctions;
- parasitic pathologies of the brain.
Most patients experience the first manifestations of epilepsy before the age of 18; at older ages, the development of the disease is much less common.
An epileptic seizure should not be confused with hysterical seizures. With the latter, vivid emotional reactions in the presence of loved ones or acquaintances become a source of pathological behavior. Also, hysterical attacks can be provoked by fear, resentment, and grief. At the same time, the person does not harm himself and is perfectly aware of what is happening. Hysteria lasts about 20 minutes, on average, while epilepsy in a one-time form never lasts more than 1-2 minutes. After a hysterical attack, a person does not feel drowsiness or stupor, unlike an epileptic one.
How to cure forever
Today, a person suffering from epilepsy is considered recovered if he has not had a seizure for five years. This is now considered to be 70% of patients.
The following factors influence the unfavorable outcome of treatment:
- incorrect treatment;
- social factors;
- late start of treatment;
- psychological state of the patient;
- the nature of the attacks.
Of course, each case must be considered individually, but based on the percentage, we can conclude that epilepsy is curable.
Are home treatments effective? Definitely yes. But only in combination with traditional medicine!
Treatment of epilepsy is a long, regular, effort-requiring process. But having the right psychological attitude, using all the variety of existing treatment methods, enlisting the support of an experienced doctor and following his recommendations, you can overcome this disease.
Symptoms of the disease and manifestations of attacks
The signs that are characteristic of the disease in question are very variable and may depend, first of all, on the area of the brain that is damaged and the extent of the disease. Temporary symptoms may also occur, for example, loss of consciousness, loss of orientation, disturbance of sensations and movements, mood, and disruptions in other cognitive functions.
Patients with seizures most often have other health pathologies, for example, bruises and injuries. They are characterized by various psychological disorders and depression. The risk of dying prematurely if you have seizures is very high. It exceeds the similar risk in healthy people by 3 times. Residents of those countries where the social standard of living is very low and there are no conditions for comfortable living have the highest risks. Also, epilepsy is more developed in rural areas compared to urban areas. The causes of death for epileptics in countries with a low standard of living are drowning, falls, burns, and prolonged seizures leading to complications and physical damage.
Stages of the disease
There are several development options for epilepsy. The disease begins with a convulsive generalized attack, which over the next years and decades does not manifest itself in any way. However, when the second case occurs, the seizures become more frequent. Sometimes the disease develops with frequent generalized seizures with high intensity of manifestations.
The second option for the development of epilepsy is the occurrence of small seizures, which gradually intensify and flow into local large convulsive seizures. Some types of epilepsy can manifest themselves for a very long time only as mild hallucinations, dizziness, and absence seizures. The intensity of development and increase in symptoms is individual in each case.
Consciousness is gradually impaired as the disease develops. At first, its disturbance is very mild, and in the end it completely leaves the person for a certain time. Seizures occur more often in men. Hallucinations and dizziness become more intense over time. In women, epilepsy has its own characteristics associated with endocrine changes of a cyclical nature. Moreover, during menstruation, all symptoms of epileptic seizures are exacerbated.
The most important manifestations of epilepsy are mental changes of a chronic and periodic nature. Periodic changes in epilepsy are represented by a variety of dysphoria or severe mood swings, expressed in anxiety, melancholy, restlessness, anger, and epileptic psychoses. Chronic changes include pedantry, thoroughness, importunity, a narrow range of interests, and egocentrism.
Status epilepticus is the most severe manifestation of this disease. With status epilepsy convulsions replace each other continuously, the patient does not have time to regain consciousness between them. This situation poses a threat to the patient’s life and requires resuscitation measures.
It is important to understand that a single seizure is not epilepsy. Only the recurrence of the disease allows us to talk about such a diagnosis. Epilepsy does not include reactive seizures that have a strong impact on a particular person. Reactive seizures include seizures that often occur during sudden changes in body temperature - febrile seizures, seizures from ingestion or insufficiency of alcohol, seizures due to sleep disturbances. If the provoking effect is removed, then the attacks will be eliminated, so they do not require specific therapy.
But treating true epilepsy is extremely important. Seizures each time damage the brain, pose a threat to human health and even life (while driving, swimming, etc.), and catastrophically reduce the patient’s quality of life, imposing certain restrictions on it. Epileptics have high psychosocial vulnerability. If the disease is not treated, it will develop into life-threatening status epilepticus.
Is a complete cure possible?
Content:
- Is a complete cure possible?
- Drug therapy
- Surgical intervention
- Neurostimulation of the brain
- Laser therapy for treatment
- Spa treatment
- Traditional medicine methods
- How to stop an attack at home
- Treatment options for children
- Consequences if left untreated
- Where to go if you have symptoms of epilepsy
In the acquired form of the pathology, epilepsy can sometimes be cured completely. However, this disease has a unique character; patients’ behavior during attacks may change significantly, which may partially complicate therapy.
In total, three types of epilepsy are known - hereditary, acquired (arising due to traumatic brain injury, inflammatory brain processes), causeless (when no cause-and-effect relationship has been identified). Benign epilepsy does not occur in adult patients; it is a childhood disease that goes away with age, even without medical intervention. However, some doctors consider epilepsy a chronic neurological disease with regularly recurring attacks and inevitable pathological consequences for brain structures.
In practice, there are often cases of the absence of a progressive course of epilepsy, when, after a long absence of seizures, patients retain optimal thinking abilities. All this indicates that there is no clear answer to the question of a complete cure for epilepsy. Severe brain damage, epileptic childhood encephalopathies, and meningoencephalitis are definitely not curable.
How effective the therapy turns out to be can be influenced by factors such as the nature of the seizures in a particular patient, the age of the patient at which the seizures manifested, and the person’s intellectual level. In this case, an unfavorable prognosis for treatment will be in such cases as:
- treatment begins untimely;
- therapy is ignored while the patient is at home;
- social circumstances not conducive to treatment;
- individual characteristics of the patient.
Diagnosis of the disease
Electroencephalography is widely used to diagnose the pathology in question. Focal “peak-wave” complexes – asymmetrical slow waves that indicate an epileptic focus and its location – are of utmost importance in diagnosis. Generalized “peak waves” indicate a high level of convulsive readiness of the brain in general and absence seizures. However, it is important to understand that an electroencephalogram does not indicate the presence of epilepsy in the body, but only demonstrates the functionality of the human brain (phases of active or passive wakefulness, sleep phase) and can show results within the normal range even in the case of frequent seizures. By analogy, the presence of epileptiform changes on the electroencephalogram does not necessarily indicate epilepsy, which means that based on this diagnostic data alone one cannot draw conclusions about the presence of the disease. But at the same time, under certain medical conditions, an electroencephalogram can become a reason for prescribing a number of anticonvulsant drugs, even without obvious symptoms and attacks.
Surgical intervention
If drug therapy for epilepsy is ineffective, doctors sometimes use neurosurgical intervention, that is, they perform surgery on the patient’s brain. The development of seizures in epilepsy is always provoked by excessive activity of some part of the brain, called the epileptogenic focus. After excitation of the epileptogenic focus, activity can spread to other parts of the brain, and the patient begins to have an attack. The goal of surgical intervention will always be to limit the spread of excitation from the identified focus or eliminate it along with part of the patient’s brain.
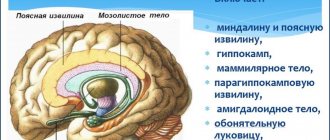
The spread of such excitation can be limited by making incisions along the surface of the brain or dissecting the corpus callosum, which is an array of fibers that serves as a connecting structure between the cerebral hemispheres. Dissection of the corpus callosum will block the path of excitation from one hemisphere of the brain to the other, which will help avoid attacks in the future. Superficial incisions along the cortex block the path of excitation to other parts of the brain, and its partial removal helps eliminate the source of the attack.
Before surgery, it is very important to accurately determine the location of the lesions. Neurosurgery for epilepsy is used without regard to the age of the patient, but it is not effective for every form of the disease or type of attack. Also, any operation may have irreversible complications with neurological disorders (for example, the patient may remain paralyzed).
In case of focal type of epilepsy, provoked by brain tumors or aneurysm, surgical treatment is indicated for the patient. Operations are most often performed without the use of general anesthesia to monitor the patient’s condition and prevent damage to the most important brain areas that are responsible for the functions of movement, thinking, and speech. Therefore, during brain surgery for epilepsy, local anesthesia is used.
Surgeries are also highly effective for the temporal form of the disease. The temporal lobe of the brain is either resected or the hippocampi and amygdala are selectively removed. The second in this case is much better for the patient, and more than 90% of such operations result in the person never having seizures again.
In case of underdevelopment of the cerebral hemisphere or hemiplegia in children, such hemisphere is completely removed through hemispherectomy. In case of primary idiopathic epilepsy, callosotomy is indicated, aimed at interrupting connections between the cerebral hemispheres and, accordingly, getting rid of seizures.
Treatment methods
In 70% of cases, drug therapy helps to get rid of epilepsy attacks. All treatment of the disease in question is divided into 2 groups - medicinal and surgical. In addition, you can additionally use physical therapy, psychological personality correction, bioacoustic correction of the brain and other techniques.
Pathology surgery is resorted to in cases where drug therapy for a long time does not bring positive results, as well as in cases of focal epilepsy, in epilepsy provoked by tumors in the brain, aneurysm, and other abnormalities in the structures of brain activity.
In patients, excitation and inhibition in the cerebral cortex are not balanced. For this purpose, physical therapy can be used, which helps stimulate the normalization of these processes. Rhythmic movements and complex breathing exercises have a positive effect on nerve cells, harmonize the mental state, and prevent stress and illness.
Objectives of conservative treatment of epilepsy
Epilepsy is usually treated conservatively or surgically. Alternative treatment of epilepsy is also possible, based on the use of leaves, roots, seeds of herbs, their infusions, decoctions, collections, bee products, etc.
Research has proven that epilepsy is 50-80% curable. Properly selected drug treatment can achieve stable remission. Newly diagnosed epilepsy with subsequent treatment after the first course of therapy in 60% of cases no longer bothered patients, or receded for 2-5 years.
The conservative method of treating the disease mainly involves taking antiepileptic drugs. Therapy goals:
- Correct differential diagnosis of the form of epilepsy and seizures, which determines the adequate selection of medications.
- Identification of the cause of epilepsy (symptomatic form) - exclusion of a structural defect of the brain (tumor, aneurysm).
- Elimination of factors that provoke seizures (alcohol, overexertion, hyperthermia, lack of sleep).
- Relief of seizure or status epilepticus. This is done by taking anticonvulsant medications (one or a combination) and providing first aid when a seizure occurs. It is mandatory to control the patency of the airway and prevent tongue biting, protecting the patient from possible injuries.
Limitations and recommendations
To excite the entire nervous system, a person only needs to drink a cup of coffee. The caffeine from this drink activates and overstimulates, among other things, neurons of the cerebral cortex that suffer from overexcitation in epileptic patients. Coffee increases the nerve impulse, which, on the contrary, needs to be reduced, and helps accelerate nerve impulses between neurons, which provokes an invigorating effect. However, an overestimation of the nerve impulses of neurons in the epileptic focus provokes a new epileptic seizure and neutralizes the effect of anticonvulsants. In addition to all of the above, drinking caffeine-containing drinks (tea, coffee, cocoa) over a long period can cause destruction of neurons in the brain, even in a healthy person.
Since alcohol has a destructive effect on the human brain and it is very often the cause of an epileptic seizure in an alcoholic, the question of the advisability of drinking alcohol for epilepsy disappears by itself. However, it is important to understand that alcoholism itself is a terrible disease, no less severe than epilepsy. Congenital epilepsy consists in the symptoms of epileptic brain readiness - in the abnormal functionality of neurons, which wears out and destroys them. When neurons die in the brain, important functional connections are interrupted, which causes degradation of the patient. Alcohol consumption provokes increased death of neurons, which leads to the loss of personal human qualities in alcoholics.
Acquired epilepsy does not occur abruptly due to a single strong libation or from periodic tiny doses of alcohol that some people allow themselves to drink; it is provoked by regular poisoning of the body with toxins of ethyl alcohol consumed in large quantities. Alcoholics with diseases of the central nervous system are dependent on alcoholic beverages, but alcohol consumption provokes accelerated personality degradation, increases the occurrence of attacks and contributes to the speedy death of the alcoholic. This is why patients with epilepsy are strictly prohibited from drinking alcohol.
When choosing a profession and future work, restrictions for patients are associated with the possibility of seizures, during which, due to their duty, they can cause harm to people around them. Such people are prohibited from driving vehicles (especially for passenger transportation, since driving a personal car is allowed in some states), working at heights, near unprotected mechanisms, bodies of water, performing military or contract service in the army or navy, being a police officer, fire brigade, prisons, security organizations, ambulances. It is very dangerous to work with moving mechanisms, chemicals, and fragile objects.
To determine the level of performance, it is necessary to determine the type of epilepsy, as well as the severity of the pathology, the patient’s concomitant diseases, the presence of intellectual or physical impairments, and the degree to which the patient can control the attacks that occur. Shift work is most often not harmful for people with epilepsy, as it allows them to get enough sleep and regularly take medications prescribed by their doctor.
Regarding driving, it is worth saying that, for example, in America, the legislation regarding people with epilepsy differs even in different states. According to statistics, road traffic accidents due to the fault of patients with epilepsy occur somewhat more often than due to the fault of healthy people, however, this incidence forms similar statistics to patients with cardiovascular pathologies and is significantly lower than that demonstrated by people who are intoxicated.
The main criterion for road safety is the time that has passed for the patient since the last attack. In a number of countries, driving a personal car is prohibited from the moment of the first epileptic seizure - in Russia, Greece, Japan, Brazil, India. In Canada and America, the patient can be allowed to drive a car if 3 months have passed since the last attack.
Most cases of epilepsy do not exclude the possibility of living in a family with people of the opposite sexes or having children. During pregnancy, it is necessary to undergo a comprehensive medical examination and be carefully monitored by a doctor all the time until the birth of the child.
Drink 1000 Skvortsova A.V.
Another remedy for the treatment of epilepsy is “drink 1000” by A. V. Skvortsova. The drug is prepared on the basis of medicinal herbs and propolis. The method for its creation was patented by Skvortsov, a physicist from the Novosibirsk academic town.
The drink acts as a general tonic and is prescribed for epilepsy because it:
- Helps improve the conductivity of impulses from the nervous system to all human tissues and organs;
- Allows you to restore strength lost during attacks and relieve stress;
- Improves all cognitive processes, especially memory;
- Increases the performance of a person with a chronic illness;
- Improves hearing, smell and vision;
- Allows you to cope with vegetative-vascular dystonia and increased intracranial pressure;
- Stimulates cerebral circulation, helps accelerate metabolic processes;
- Suitable for the prevention of cardiovascular diseases, which are frequent companions of epilepsy. Reduces the risk of stroke and minimizes its consequences.
Contraindications include only individual intolerance to the components included in the drink. The substances from which this product is made include propolis, extracts of St. John's wort, nutmeg and thyme, as well as the biological additive Alpam 7. The drink should be given to children under 7 years of age with caution.
There is a certain method of application and dose that should be followed by patients with epilepsy:
- For adults (the dosage is also suitable for children over 7 years old), 10 drops are recommended. Better during main meals;
- For infants under 12 months of age, 1 drop should be diluted with water (20 ml). Give by teaspoon. You should take no more than 4 spoons per day;
- For children over 1 year old and under 7 years old, the calculation is 1 drop for each year lived. The number of doses is the same as for adults.
For ease of use, the drug is available in an unbreakable plastic bottle equipped with a dispenser. The bottle contains 30 ml of drink. It is important to use the product completely after opening the bottle within 2 months. The total shelf life of a sealed drink is 3 years. It is stored in a cool, dark place. If a sediment is found upon opening, this is considered normal. The main thing is that before counting the drops, do not forget to shake the product well.
Where can I buy?
“Drink 1000” can be purchased in the name of Skvortsov in Vladivostok, or delivered by mail through the official website.
Nutrition for illness
Doctors have not recognized a single diet plan for epilepsy. The fact is that some theoretically permitted food products can provoke migraine attacks in patients, so they must be privately excluded from the menu. If diabetes occurs in parallel, the patient may experience new seizures when consuming sugar-containing foods. Dairy-vegetable foods are often recommended for such patients, but meat and other proteins cannot be excluded from the menu. This rule is important to follow when consuming hexamidine, which affects general protein starvation. When consuming protein, you need to eat boiled meat and fish in equal quantities.
If a patient takes medications for a long time, he begins to lack folic acid, homocysteine, and vitamin B12. If this need is not met in a timely manner, the patient may develop schizophrenic complications.
The ketogenic diet is effective for epilepsy, in which the patient’s diet should combine 1/3 proteins and carbohydrates with 2/3 fats. This diet is highly effective in treating children. After hospital treatment and three days of fasting, this diet is recommended for children. If the body perceives it normally for several days, the patient can then most often be transferred to a normal diet.
If anticonvulsant therapy is ineffective, doctors recommend following a fasting diet. The fact is that people with epilepsy always experience improvements when they fast or go on long periods of fasting, but this method of therapy can only be used for a limited time. Supplying the body with vital nutrients is essential for any disease.
The patient's diet should be varied. It should contain foods rich in fiber, fruits, and vegetables. They create conditions for normal intestinal motility, preventing constipation. If you have epilepsy, it is not recommended to have dinner later than 2 hours before bedtime.
How to improve your health at home
Epilepsy is a serious disease, can it be effectively cured using home recovery methods? Is it realistic or not to improve the condition of the body using traditional medicine?
The benefits of such treatment have been proven by many specialists.
Rock oil, which contains a huge amount of useful elements, is very useful. You will strengthen your health and also improve your immunity.
The antispasmodic effect perfectly combats the symptoms of epilepsy. Preparing the medicine is quite simple; dilute one and a half grams of oil in one liter of water. Take a glass of this tincture three times a day
The folk method is effective if you use powder from several herbs. Take peony and duckweed and then grind them with a coffee grinder.
A teaspoon of the mixture should be washed down with a sufficient amount of water. The course of treatment should be completed in two weeks, only after some time has passed, repeat this process.
Maryin root is an effective assistant in the fight against epilepsy. The remedy is also used for paralysis and neurasthenia. Prepare a special tincture with alcohol (let the plant brew for several days).
The smell of myrrh is another beneficial remedy that will help improve your health. The patient's room should smell the substance. This method is often recommended for people who suffer from neurosis.
to contents ^
Living with epilepsy
Death
Early mortality in patients with the disease in question is not uncommon. In almost half of the cases, mental disorders that arose as a result of the disease are to blame. The main causes of death are suicide and injuries that people receive during attacks.
Lifespan
Life expectancy in patients with epilepsy is shorter than in healthy people, since with this pathology there is a high risk of other pathologies as complications. Very often such complications include chronic pulmonary pathologies, cardiovascular problems, and neoplasms in the human brain.
Russian experts do not consider injuries from falls in the event of an attack or suffocation during this period as the main causes of early death. In severe pathological conditions, on the eve of seizures, patients experience a period of aura - a set of symptoms warning of the onset of an attack. That is why a person can always take measures to prevent various injuries.
Neurostimulation of the brain
If the epileptogenic focus is located in a certain area of the brain without movement, neurosurgery can be used. For drug-resistant epilepsy, this method is not suitable due to the multiplicity of constantly wandering lesions. In this case, doctors use the technique of neurostimulation of the vagus nerves.
The vagus nerves help the brain control the functioning of the internal organs of the abdomen and chest cavity - the heart, lungs, stomach, and parts of the intestines. The nerve is paired and runs down the left and right sides of the neck from the brain. It is necessary to influence the vagus nerve on an ongoing basis using special equipment similar to a pacemaker. Stimulation electrodes are attached to the nerve on the left and the pulse generator is placed subcutaneously. After implantation, the patient contacts the doctor to adjust the pulse frequency and monitor the condition of the device.
The method of vagus nerve stimulation has been used in the treatment of drug-resistant epilepsy for decades, but the clear mechanism of action of such treatment is not yet completely clear. However, clinical data support the benefit of this technique in children and adult patients whose epilepsy is resistant to drug treatment. Neurostimulation can also be used in combination with drug therapy if the latter is insufficiently effective or if surgical intervention is ineffective or impossible.
How dangerous is the disease?
Best materials of the month
- Why you can't go on a diet on your own
- 21 tips on how to avoid buying stale food
- How to keep vegetables and fruits fresh: simple tricks
- How to curb your sweet cravings: 7 unexpected products
- Scientists say youth can be extended
Mild forms of epilepsy have virtually no effect on the normal course of life of patients, since seizures in such cases are extremely rare, and brain cells are not subject to rapid destruction. In severe types of the disease, generalized attacks often occur, lasting from 30 to 40 minutes. These periods can make a person helpless, since they provoke disruptions of the entire body, and breathing may stop.
If patients do not have secondary pathologies, the main danger for them will be various falls. Not every patient is able to recognize the aura, which can result in injury and injury. This is the reason for limiting certain types of work and driving.
Encephalopathy of an epileptic nature in young children can lead to impaired cognitive functions and changes in behavioral reactions. In children, memory deteriorates, concentration and brain activity decrease, and sudden changes in mood may begin.
Living with epilepsy is not easy, but to alleviate the condition, social and personal adaptation and acceptance of your illness are required. If you follow all medical prescriptions, you can live a full life, work, build a family and deny yourself virtually nothing.