Delirium is one of the most common types of confusion. This transient mental disorder is of an exogenous nature and develops as a result of functional disorders of the brain against the background of severe intoxication and disease. Therefore, treatment of delirium is aimed not only at relieving the main psychotic symptoms, but also at correcting primary disorders.
Delirium: what's behind the name?
The name of the disease comes from the Latin delirium - “delirium, madness.” The essence of the disease fully corresponds to these concepts. Attacks of delirium in mentally ill people have been studied in ancient times, BC.
Delirium belongs to the so-called psychotic disorders, in which the patient’s consciousness can be impaired to varying degrees. Initially, scientists paid attention only to obvious signs of deviations in the state of consciousness: delusional ideas, muttered speech, inadequate reactions, causeless movements, etc.
As medicine has advanced, the concept of delirium has expanded. Subtypes of the disease include reversible delusional states of various etiologies. A large group of provoking factors consists of diseases of a nervous, infectious, viral and other nature. There is also the most common popular idea of delirium - such a variety as “delirium tremens” in chronic alcoholics. There are actually many types of delirium. The disease can be somatogenic in nature and affect people who do not drink at all.
If the disease has progressed far, the patient may pose a danger to himself and others, even threatening health and life.
Establishing diagnosis
Diagnosing delirium in itself is not particularly difficult. It is much more difficult to determine the cause that provoked this condition. First of all, delirium is differentiated from psychosis, which occurs without disturbances of consciousness, and from senile dementia.
The doctor collects a complete medical history of the patient. For this purpose, the patient’s relatives are interviewed about the circumstances under which confusion arose, whether the pathology was preceded by the use of drugs and medications, as well as alcohol, how quickly this condition progressed and what the psychological and physical state of the patient is.
Next, after collecting an anamnesis, a full examination is carried out, in which the patient’s neurological reactions are of particular importance. Among the diagnostic methods:
- blood analysis;
- X-ray examination;
- lumbar puncture to obtain cerebrospinal puncture.
Etiology of the disease
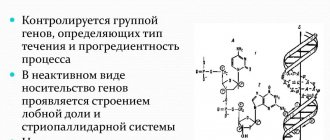
The mechanism for the development of delirium is based on a violation of the neurotransmitter functions of the cerebral cortex and subcortex. The transmission of nerve impulses from the brain slows down, which manifests itself in a number of symptoms. Two conditions become the impetus for changes to occur: brain hypoxia and brain intoxication. In conditions of lack of oxygen, metabolic processes in the brain tissue are disrupted, as a result of which toxic substances are concentrated in the cells. Neuroinflammation may occur.
Delirium usually represents a somatic pathology. A number of organic factors can act as its root causes:
- Systematic long-term alcohol consumption;
- withdrawal delirium after abrupt cessation of use;
- dangerous infectious diseases accompanied by fever and fever (typhoid fever);
- acute respiratory viral infections with a strong degree of intoxication (influenza, pneumonia);
- streptococcal infections;
- pathologies of medium and small blood vessels of the brain in cardiovascular diseases;
- infectious lesions of the nervous system with changes in the tissues of the brain and blood vessels.
- rheumatic diseases;
- diseases of protozoal nature (malaria).
The risk of delirium exists in conditions of severe immunodeficiency, including AIDS, as well as heart attacks, strokes, and acute gynecological inflammation. An attack of the disease can be caused by acute inflammatory processes in the intestines, requiring surgical operations: appendicitis, peritonitis, intestinal obstruction. In addition, delirium is not excluded in diseases with any failure of internal organs (renal, cardiac, liver).
The list of provoking causes includes states of deep, severe anesthesia during surgical operations.
Weak immunity, dehydration, chronic diseases, simultaneous use of many medications, as well as old age and chronic stress are all additional risk factors. But even if a person is completely healthy and young enough, no one guarantees that a severe infection will not cause such a complication.
Typology of disorders of consciousness
Disorders of consciousness are extremely heterogeneous, ranging from inhibition to excitation [18], in extreme cases of inhibition at times approaching comatose states, and in extreme cases of excitation resembling schizophreniform psychoses. Cognitive disorders also vary in severity, including both forms of cognitive impairment that are limited to attention disorders and forms with transient “focal” cognitive deficits.
Psychiatrists who have studied the clinical features of somatogenic psychoses have described a variety of manifestations of disorders of consciousness. In a systematic analysis of symptomatic psychoses, K. Bonhoeffer [19] distinguished delirious, amental and twilight disorders of consciousness. Following him, E. Kraepelin [20] mentioned delirium and amentia as manifestations of parainfectious psychoses. In later classifications, amentia could be classified as a type of delirium [4], which was confirmed by early observations that identified forms of delirium with more pronounced cognitive fragmentation [19]. Recent work conducted with the participation of a contingent of elderly patients in a multidisciplinary hospital [21] revealed several types of confusion, including delirium (37.9%), amentia (18.7%) and forms of confusion with confabulation (11.8%), approaching Korsakov's syndrome.
Despite the fact that the boundaries between different types of disorders of consciousness are blurred, the creation of a clinical typology has not only scientific, but also practical value. First, it equips the researcher with a more sensitive diagnostic tool that can capture individual differences while at the same time integrating them into delineated nosological units. Secondly, attention to various clinical manifestations allows us to evaluate their prognostic significance.
Another trend (and so far the prevailing one) is to follow the syndromic and statistical classification, which, without making a nosological distinction, combines a variety of post-stroke clouding of consciousness into the group F05.x “Delirium not caused by alcohol or other psychoactive substances” [22]. But even with a syndromic approach, clinical needs force us to consider syndromes that go beyond the usual somatogenic psychoses: for example, evening confusion in patients with dementia [23, 24].
Although foreign works do not distinguish between delirious, oneiric and amentive disorders of consciousness, such a distinction is of great practical importance, since different syndromes may have different etiologies and prognosis. Thus, delirious and oneiric symptoms are often found in infectious-toxic diseases [25].
The creation of a clinical typology for patients with brain damage primarily pursues a pragmatic goal - to distinguish disorders directly related to damage to certain structures from disorders the appearance of which is caused by secondary factors (biochemical post-ischemic cascade or intoxication of a somatic nature).
In this regard, the approach of the Russian neuropsychiatric school, which is used to classify the consequences of traumatic brain disease, is interesting [26]. The authors separate the syndromes of stupefaction (delirium, oneiroid, twilight changes in consciousness) from various forms of confusion (amnestic, amnestic-confabulatory, speech, etc.). The presence of confusion reflects predominantly the disintegration of cognitive functions (and certain damage to brain structures), while delirium and oneiroid are manifested by disorientation, closely associated with hallucinatory-delusional symptoms (and secondary toxic brain damage).
Main signs of delirium
Delirium fully justifies its characterization as clouding of consciousness. He is accompanied by:
- Nightmarish dreams;
- difficulty perceiving the real world;
- amnesia;
- violation of orientation in space, time;
- disturbance of mental activity;
- hallucinations;
- states of affect of fear, anxiety;
- attempts to protect yourself from the imagined “danger”;
- periods of psychomotor agitation or, conversely, complete immobility;
- bouts of aggressiveness.
Symptoms depend on the type of delirium and its course. Some of the mentioned manifestations may not be observed at all.
Stages of development of delirium
Delirium is a mental disorder that develops gradually. Each stage of the disease has its own special symptoms:
- The first stage is not always noticed by others and the patient himself. Only precursors of the disease, pre-delirium symptoms, are observed. The person becomes more talkative, experiences vivid memories of the past, and thinks in unexpected associations. The level of critical thinking decreases, orientation is disrupted. During this period, sleep disturbances often occur, and the sleep and wakefulness patterns are disrupted. If a person is sleeping, he wakes up very easily. Characterized by vivid, very “real”, believable dreams.
- At the second stage, attention deficits, difficulties with concentration, and sober perception of reality increase. It becomes difficult for a person to navigate in time. The first precursors of hallucinations appear - visual illusions. Moreover, when you try to take a closer look at the apparent phenomenon, it does not dissipate, but becomes clearer. Fear grows from imaginary dangers.
- The third stage is characterized by the beginning of real hallucinations. The patient's attention is switched to these visions. Most often these are visual images, but there can be auditory and tactile sensations. Human behavior begins to obey this augmented (or parallel) reality. He can lie in bed and tear the bed linen, move in panic, shake off apparent insects, and barricade the entrance to the home. At such moments, the patient can be dangerous both for others and for himself due to inappropriate actions. These include the use of physical force, aggression, going out onto a busy roadway, jumping out of a window on any floor, etc. It is extremely difficult to conduct a dialogue with a person in such a state. He ceases to navigate in space and has difficulty determining his location. Difficulties falling asleep and a shift in sleep patterns from night to morning are also typical.
Delirium tremens
Alcoholic delirium is popularly called “delirium tremens.”
It occurs against the background of excessive and prolonged abuse of alcohol.
It occurs at stage III or even stage II of alcoholism during the period of complete cessation of drunkenness.
In this case, the pathology is characterized by such symptoms as:
- unconscious delusion;
- hallucinations;
- chills;
- increased body temperature;
- headache;
- vomit;
- tremor;
- a state of severe anxiety;
- sleep disturbance, as a rule, nightmare visions occur;
- after a few days, insomnia may occur, which is accompanied by vivid hallucinations.
Delirium occurs not against the background of intoxication itself, but as a result of the abolition of the usual intake of alcoholic beverages, on the second or even fifth day. The hallucinations that accompany delirium delirium are menacing in nature, and the patient experiences a strong sense of fear. He can see fabulous fantastic creatures, hear voices addressed to him, or, on the contrary, not concerning him.
Along with this, attacks of paranoia are noted, that is, a person constantly thinks that someone is watching him, that his life is in mortal danger.
A fever can last from two to five days, but in the case of any concomitant disease, the disorder may not stop for several weeks.
In the daytime, as a rule, the attacks pass, the patient’s condition improves, consciousness clears up, the person becomes adequate and can even describe everything that happened to him during the attack. In moments of enlightenment, he realizes that he is sick. As evening approaches, the psychosis returns.
A patient with alcoholic delirium requires urgent hospitalization. Treatment takes place in a psychiatric or drug treatment clinic, where body detoxification procedures and maintenance drug therapy procedures are used. The main sign that the patient is recovering is the complete normalization of sleep.
Alcoholic delirium is a very dangerous condition in which the patient poses a serious danger to others and to himself due to uncontrolled attacks of aggression. What could be the possible outcome of such a condition:
- full recovery;
- subjective recovery with a defect in the intellectual sphere;
- death - in the absence of qualified treatment.
What is delirium like?
Delirium is divided into several main types:
- Classic or typical.
- Hypokinetic – characterized by the absence of deviations in behavior and a tendency to apathy and physical inactivity; can be confused with depression or asthenic syndrome.
- Mumbling (mussing) - sometimes classified as the fourth stage of delirium; is distinguished by complete detachment from reality, muttering, making small fingering movements followed by amnesia. Severe delirium.
- Professional - is also considered a severe form of mental confusion, although there may not be hallucinations. The patient constantly repeats monotonous movements associated with professional activities (driving nails, typing, knitting, sewing, sawing boards, etc. activities using motor skills).
- Abortive type (with or without hallucinations).
- Alcoholic (delirium tremens) – develops after leaving the binge; the patient sees non-existent insects, animals, people. The dominant hallucinations may be verbal or visual. It is divided into typical and atypical subspecies.
Delirium is also classified by severity. Delirium with a fatal outcome is separately distinguished, which includes any type with the possibility of death of the patient.
Types of violation
Delirium is divided into the following forms:
- abortive - transient, in which the symptoms are not clearly expressed;
- acute - develops intensively, characterized by vivid manifestations;
- prolonged - lasts a long time, memory and criticality are preserved, hallucinations mainly occur at night.
Delirium caused by various factors can be:
- alcoholic;
- withdrawal symptoms;
- atropine;
- hypnagogic - appears at the moment of transition from sleep to wakefulness;
- infectious;
- hysterical - reaction to psychogenic-traumatic stimuli;
- narcotic;
- medicinal;
- febrile - at elevated temperatures;
- vascular;
- age - accompanies senile dementia;
- toxic;
- traumatic.
In addition, delirium varies in clinical manifestations:
- auditory - auditory hallucinations predominate, more often observed in alcoholism disorder;
- mumbling - accompanied by unintelligible muffled muttering, repetition of simple movements;
- oneiroid - occurs as a result of psychotic disorders, characterized by a variety of vivid hallucinations;
- delirium of siege is one of the types of alcoholic in which a person experiences fear due to hallucinations and tries to hide or otherwise protect himself;
- professional - the patient makes movements that he performs in a working environment;
- furious - accompanied by intense psychomotor agitation and aggression;
- schizophrenoid - accompanied by schizophrenia-like symptoms;
- epileptic - occurs after the end of an epileptic attack.
Principles of treatment
Treatment of delirium should be comprehensive. Antipsychotics are used only to relieve severe symptoms. They are not prescribed as a prophylactic agent. The doctor’s choice of drug depends on the severity of delirious symptoms. In severe cases, haloperidol, stelocin, triftazine, chlorprothixene and others help. Neurodeptics with a sedative effect, such as carbidine, azaleptin, can be prescribed.
In case of post-anesthesia (postoperative) delirium, it is necessary to provide the patient with peace and minimize stress. After the final recovery from anesthesia, consciousness will be restored.
One of the goals is to maintain water-salt balance in the body. It is important to restore normal metabolic processes at the cellular level. Antidotes are also used for intoxication. Reosorbilact, trisol, glucose solution, isotonic solution may be prescribed.
If the cause of the disease is an infection, it is treated. The same goes for any other disease. The high temperature goes down. Antiviral agents are used: Tamiflu, Amizon, Odeltamevir and others.
For cerebral ischemia, medications are prescribed to improve blood supply to brain tissue. Sedatives and hypnotics may also be prescribed. They are taken in the evening to correct the patient's sleep and wakefulness patterns.
If the patient does not undergo treatment in a hospital, the results of treatment are secured by taking tranquilizers prescribed by the doctor (tazepam, nitrazepam, mebicar, etc.).
Careful monitoring of the patient's behavior is required, especially in the third stage of the disease during seizures.
Prevention
To prevent delirium in older adults during a hospital stay, family members can ask hospital staff for help by doing the following:
- Ask the patient to walk around the room regularly.
- Bring a clock and calendar to the room.
- Minimize sleep interruptions and noise during the night.
- Ensure that the patient eats and drinks enough.
Family members can visit and talk with the patient, maintaining ongoing awareness. Patients with delirium may be afraid, but the familiar voice of a loved one can be calming.
Forecast
Delirium is not a life-threatening condition, except in cases of particularly severe confusion with characteristic disorientation. However, if the disease is not treated, in later stages it threatens to develop into more dangerous conditions. In particular, there are known cases of transformation into oneiroid, a condition accompanied by mystical hallucinations.
Most patients with delirium are completely cured. Recovery takes longer in older patients with multiple chronic diseases. For such people, this may take weeks or months. Some of these patients are not able to restore brain function to its original state.
During the first two years after treatment for delirium, the risk of functional and cognitive impairment remains. It is necessary to pay enough attention to health and undergo periodic examinations in order to prevent possible complications in time. In advanced cases, there is a danger of consequences in the form of organic diseases.
General information about the disease
Delirium is a sudden, intermittent, and usually reversible disturbance of mental function. This disorder is characterized by an inability to focus, disorientation, inability to think clearly, and fluctuations in the level of perception (consciousness).
Delirium is a pathological mental disorder, not a disease. Although the term has a specific medical definition, it is often used to describe any type of confusion.
Delirium is never a normal condition and often indicates a usually serious, recently developed pathology, especially in older people. People with the disorder need immediate medical attention. When the cause of delirium is identified and quickly treated, the disorder is usually curable.
Because delirium is a temporary disorder, it is difficult to determine the extent of the disorder in the population. Delirium affects 15–50% of hospitalized patients aged 70 years and older.
Delirium can occur at any age, but is most common in older people. Delirium is common among nursing home residents. When the disorder occurs in younger people, the cause is usually drug use or a life-threatening illness.