Cognitive functions are the cognitive tools of the brain. Every day a person receives information, the brain processes it, translates it into knowledge and life experience. Cognitive functions include attention, perception, imagination, thinking, memory, intelligence, speech, etc. All this depends on the active ability of the brain and general health.
The first symptom of cognitive impairment is forgetfulness.
What is cognitive impairment
Cognitive functions are perception, intelligence, the ability to get acquainted with new information and remember it, attention, speech, orientation in space and time, motor skills. Over time, a person begins to experience disturbances in everyday behavior due to disruptions in cognitive functions. Isolated cases of forgetfulness are not a reason to worry, but if a person begins to regularly forget events, names or names of objects, then this may indicate disturbances in brain activity, then the patient needs the help of a neurologist.
Cognitive distortions
Cognitive distortion is a person’s irrational thinking and systematic errors in judgment. They arise due to the individual’s strong beliefs and faith in something, stubbornness and inability to give in and admit a mistake. Marketers and psychics readily use this:
- It is human nature to imitate others, that is his nature. If the majority buys a certain product or believes that a black cat brings trouble, an individual with a cognitive distortion will accept these facts on faith.
- The “anchor” effect is also triggered - an association associated with a certain phenomenon.
- The halo effect, when a certain opinion begins to cover everyone around one by one, for example, an approving review of someone by a television star, which will be listened to by tens, hundreds of people.
Symptoms
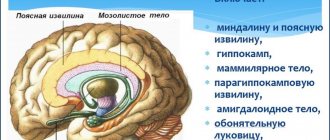
If the impairment of cognitive functions is associated with the left hemisphere of the brain, then one can observe such external symptoms as the patient’s inability to write, count, read, difficulties with logic and analysis begin, and mathematical abilities disappear. The right hemisphere affected by the disease will produce spatial disturbances, for example, a person ceases to navigate in space, the ability to dream, compose, fantasize, empathize, and engage in drawing and other creative activities disappears.
The activity of the frontal lobes of the brain is associated with the perception of smells and sounds, with the emotional coloring of the surrounding world, it is responsible for experience and memorization. If the disease affects the parietal lobes of the brain, then the patient loses the ability to purposefully perform actions, he does not distinguish between right and left, and cannot write or read. The occipital lobes are responsible for the ability to see color pictures, analyze, recognize faces and objects. Changes in the cerebellum are characterized by inappropriate behavior and speech impairment.
Mild cognitive impairment
It can be considered the initial stage in a chain of disruptions in higher brain activity, which for the most part relate to the patient’s memory. Mild types of disorders can be provoked not only by age-related changes. Often the cause is encephalitis or head trauma. What is a cognitive disorder and how does it manifest itself externally? These include severe fatigue during mental activity, the inability to remember new information, confusion, difficulty concentrating, and problems in performing purposeful actions.
It is often difficult for a patient to understand someone else’s speech or choose words to convey thoughts. An interesting fact is that this is a reversible process. With strong mental stress, the symptoms progress, and after a good rest they disappear. However, there is a need to visit a neurologist and therapist, who will conduct the necessary instrumental studies and prescribe tests.
Mild cognitive impairment
When the functioning of several processes deteriorates beyond the normal range of the patient's age, but does not reach the level of dementia, we can speak of a moderate impairment. According to medical statistics, such symptoms can occur in 20% of people over 60 years of age. However, most of these patients develop dementia within the next five years. In 30% of people, the disease progresses slowly, but if a disorder of several cognitive functions occurs in a short period of time, then urgent consultation with a specialist is necessary.
Severe form
The prevalence of dementia is observed in elderly patients, and it is usually provoked by Alzheimer's disease. AD is a brain disease associated with the death of acetylcholinergic neurons. Its first signs are loss of memory, constant forgetfulness of life events. At the next stage of progression of pathological changes, disorientation in space begins, the person loses the ability to express his thoughts, speaks nonsense, becomes helpless in everyday life and may need help from loved ones.
Often, severe impairment of cognitive functions is provoked by cerebrovascular insufficiency, then memory for life events may remain good, but intelligence suffers. Patients stop distinguishing and seeing similarities between concepts, their thinking slows down, and difficulty concentrating appears. In addition, the person experiences an increase in muscle tone and a change in gait. If such signs occur, a neuropsychological examination is prescribed.
The essence of the problem
Cognitive refers to the most complex brain functions associated with:
- the process of rational cognition of the surrounding world;
- purposeful interaction with accessible objects, phenomena and living beings;
- perception (collection, receipt) of information;
- processing and analysis of received data;
- memorization and storage in memory;
- exchange of information;
- construction and consistent implementation of sequential actions, evaluation of their results.
The ability to cognition is “trained” from infancy
Thus, cognitive impairment is associated with a decrease in these functions relative to the initial level (individual norm).
Note! Each person has his own level of development of cognitive abilities, determined by genetic characteristics. So, some can boast of a phenomenal memory, while others have difficulty memorizing simple quatrains. There are no generally accepted norms for assessing cognitive function.
There are more than twenty pathologies accompanied by impaired cognitive functions. Vascular diseases occupy an important place among them.
Common causes of cognitive decline include:
- ischemic stroke (infarction) of the brain of certain localizations (see Cerebral vascular infarction: consequences and complications);
- multi-infarction condition;
- chronic ischemia of nervous tissues – discirculatory encephalopathy, vascular dementia;
- consequences of subarachnoid or intraventricular hemorrhage;
- dysmetabolic (mixed vascular-dysmetabolic) encephalopathy - hepatic, renal, hypoglycemic, etc.
Significant thinking disorders occur after a stroke
Unfortunately, most chronic vascular diseases cause irreversible impairment of cognitive function. In some cases (for example, with successful treatment of acute cerebrovascular accident, correction of metabolic disorders), their complete or partial recovery is possible.
Causes
Violations are divided into two types: functional and organic. Functional disorders are provoked by emotional overstrain, stress, and overload. They are typical for any age and when the causes are eliminated, as a rule, they go away on their own. However, there are times when the doctor decides to use drug therapy.
Organic disorders are provoked by changes in the brain under the influence of a disease. As a rule, they are observed in old age and are stable in nature. Modern medicine offers productive ways to solve this problem, allowing you to get good results. The following reasons for violations can be named:
- Insufficient blood supply to brain cells. This includes diseases such as cardiovascular pathology, stroke, hypertension. A person must monitor his blood pressure, maintain optimal sugar and cholesterol levels.
- Age-related brain atrophy or progressive Alzheimer's disease. In this case, the symptoms of the disease increase gradually over many years. Adequate treatment will help improve the patient’s condition and stabilize symptoms for a long time.
- Metabolic problems.
- Alcoholism and poisoning.
- Cardiovascular failure.
In children
The practice of childhood neuralgia shows that cognitive deficits appear as a result of diseases affecting the nervous system of a small patient. This could be, for example, a birth injury or intrauterine infection, or congenital metabolic disorders in the child’s nervous system. There is a problem with quick and correct diagnosis, but the sooner specialists identify the disease and begin adequate therapy, the better the result will be.
Cognitive disorders in old and senile age
In older patients, the brain experiences a lot of changes, and its mass decreases significantly. This process begins early, at the age of 30-40, and by the age of 80 the degree of neuron loss can be up to 50% of the total mass. Surviving neurons do not remain the same; they undergo functional changes. On the external plane, this can also manifest itself in the form of impaired cognitive functions.
Cognitive dysfunction in older people is expressed in excessive irritability, touchiness, limited thinking, and poor memory. Their mood often changes, qualities such as pessimism, fear, anxiety, dissatisfaction with other people appear, and social and everyday disadaptation is possible. Without treatment, catastrophic cognitive impairment will result.
How to recognize cognitive impairment and dementia in older people?
Advances in modern medicine have led to increased life expectancy. According to Rosstat, in 2020, out of 146.7 million people in the Russian Federation, every fourth person (37.9 million people) was over the working age. According to WHO forecasts, the world population over 60 years of age is expected to exceed 2 billion by 2050. Thus, older people will make up 22% of the world's population. Experts note that along with increasing life expectancy, older people are experiencing an increase in non-communicable diseases, including dementia.
There are three groups of pre-dementia cognitive disorders (CD): subjective, mild and moderate. Subjective cognitive impairments include complaints from an elderly person about severe forgetfulness, decreased concentration, increased fatigue during mental work, difficulties in choosing the right word in a conversation, but the doctor does not detect any changes during neuropsychological testing. This is followed by mild cognitive impairment, identified by a specialist during a neuropsychological study, but which cannot be noticed during a normal conversation. Moderate cognitive impairment (MCI) is already noticeable to others, but a person’s professional, social and everyday activities are not yet limited. Moderate cognitive impairment occurs in 20% of people over 65 years of age. Alarmingly, among those diagnosed, 70% develop dementia within five years. Any limitation in the patient's daily activities indicates dementia. To explain what dementia is, it is the designation of a syndrome that develops mainly in chronic or progressive diseases of the brain, in which many higher cortical functions are impaired, including memory, thinking, understanding, speech, orientation, numeracy, cognition and reasoning. It is important to know that Alzheimer's disease is the most common cause of dementia, accounting for up to 60-70% of all cases. Vascular dementia, progressive supranuclear palsy, dementia with Lewy bodies, and frontotemporal degenerations are also common.
In addition to the above diseases, dementia can develop after various injuries and infectious diseases of the brain, with chronic alcoholism and metabolic disorders.
The costs of caring for a patient with dementia associated with the provision of medical and social assistance significantly affect the financial situation, quality of life and health status of members of the entire family.
Most often, it happens that the first - early stage of dementia (the first year or two) often goes unnoticed. Relatives and friends perceive it as “senility” or a normal part of the aging process. Because the disease develops gradually, it can be difficult to pinpoint when it begins.
How to recognize the first – early stage of dementia?
At this stage, patients become forgetful, especially about events that have just happened, some people may experience difficulties in communication, for example when choosing words, lose orientation in a familiar area, lose awareness of the passage of time, including time of day, month, year, season. Some older people have difficulty handling their money, as well as performing complex household chores. Some may become less active and motivated and lose interest in activities and activities, may exhibit mood changes including depression and anxiety, and may sometimes react overly irritably or aggressively
What are the signs of the middle stage of the disease?
Most often, from the second to the fourth or fifth years, as the disease progresses, signs and symptoms become more obvious and increasingly limiting a person’s capabilities: patients show severe forgetfulness, especially regarding recent events and names of people, have difficulty assessing time, date , places and events, may become disorientated in the home or community, have increasing difficulty communicating (speech and understanding), need help with personal care (toileting, bathing, dressing), unable to cope with cooking, cleaning or shopping , to living safely alone without help. In addition, changes in behavior may include walking aimlessly, repeating the same questions, shouting, obsessiveness, sleep disturbances, and hallucinations (auditory and visual perceptions of something that does not really exist). Some older adults may exhibit inappropriate behavior at home or in the community (eg, disinhibition, aggression).
What may indicate late stage dementia?
The fifth and subsequent years are a stage of almost complete dependence on other people and lack of activity. Memory impairment becomes significant and physical signs and symptoms become more obvious. At this stage, patients are usually disoriented in time and space, have difficulty understanding what is happening around them, are unable to recognize relatives, friends and familiar objects, cannot eat without assistance, and may have difficulty swallowing. Increased need for assistance with personal care (bathing and toileting), possible involuntary bowel movements and urination, difficulty moving, the patient may lose the ability to walk or be confined to a wheelchair or bed, changes in behavior may increase and include aggression towards the face caregiver, nonverbal agitation (kicking, hitting, high-pitched screams or moans), inability to navigate the house.
The growing burden on the budget of each family and states in general has gradually turned the fight against dementia into one of the priorities of WHO. Due to the lack of effective treatment for cognitive impairment at the stage of dementia, considerable attention is paid to the early detection and treatment of mild and moderate cognitive impairment (MCI). The main goal of treatment is to prevent the increase in cognitive impairment and prevent or delay the onset of dementia, as well as reduce the severity of existing impairments in order to improve the quality of life of patients.
Currently in the republic, under the leadership of the chief physician of the State Autonomous Institution of the RS (Yakutia) RCH No. 3
, Doctor of Medical Sciences, chief freelance geriatrician of the Far Eastern Federal District, RS (Y), excellent health worker of the Russian Federation, RS (Y) Olga Viktorovna TATARINOVA, identified priority ways for the development of geriatric neurology. For the purpose of early detection of cognitive impairment and dementia in the elderly, it is planned to open a memory room, the main tasks of which will be to provide treatment and advisory assistance to patients with cognitive disorders (CD), preventive (organizational and methodological) work to prevent CD in elderly and senile people . In addition, the work of primary care doctors, medical specialists, social protection authorities will be coordinated, and patient routing will be carried out, taking into account the individual characteristics of his condition. In the Department of Geriatric Neurology of the Geriatric Center of the State Autonomous Institution RS (Y) RCH No. 3, work is underway to provide specialized neurological care to elderly and senile patients, differential diagnosis and treatment correction. Under the guidance of scientific consultant, Ph.D., neurologist-parkinsologist Alexey Alekseevich TAPPAKHOV, modern achievements in the field of diagnosis and treatment of neurodegenerative diseases with cognitive disorders, such as Alzheimer's disease, multiple system atrophy, Parkinson's disease, progressive supranuclear palsy, dementia, are being introduced into practice. with Lewy bodies, frontotemporal degenerations, etc., research work is being carried out.
The department also plans to open beds for the second stage of rehabilitation of post-stroke patients. To diagnose neurological diseases, ultrasound of the brachiocephalic arteries, X-ray CT, MRI studies, densitometry, pharmacogenetic tests for statins, anticonvulsants are performed, new research methods have been introduced, such as video-EEG monitoring, ENMG, tremorography at the NEFU MI clinic, lumbar puncture (unloading test ) for hydrocephalus, neuropsychological testing. As an auxiliary type of therapy for elderly patients, the Geriatric Center provides neurobics and dance therapy.
In conclusion, I would like to say a few words about the prevention of dementia. The development of dementia, in particular Alzheimer's disease, is determined by genetic factors. But there are many modifiable risk factors that a person can influence. Firstly, this is high blood pressure from a younger age, since untreated arterial hypertension increases the risk of developing dementia by 4-5 times. Along with blood pressure levels, it is necessary to control your weight, sugar and cholesterol levels, eliminate smoking and alcohol abuse. As you can see, many risk factors for developing dementia are identical to risk factors for developing cardiovascular diseases, including stroke, which increases the risk of developing dementia by 5–10 times. A diet with a high intake of fresh vegetables, fruits, grains, legumes, nuts and olive oil, a moderate intake of fish and seafood, dairy products and a low intake of meat and sweets (Mediterranean diet) will help control these risk factors. It is also recommended to drink red wine, no more than 1 glass, vitamins B12, B6, B3, C, folic acid. Regular exercise in healthy older adults, at least 3 times a week, may delay the onset of age-related cognitive decline and also reduce the risk of developing Alzheimer's disease. Daily walking, at least 30-40 minutes, Nordic walking with poles classes, neurobics, dance therapy and other types of physical activity are recommended. Other risk factors include hearing loss, depression, low education, social isolation and lack of cognitive activity. Long-term feelings of loneliness negatively affect a person's mental health and are a risk factor for the development of both depression and dementia. Connecting with loved ones, friends and acquaintances, and participating in activities of common interest can reduce the risk of developing dementia. Intellectual activities such as reading, board games, crossword puzzles, and playing musical instruments can slow down the onset of the disease or mitigate its development.
If you have relatives in your family who suffer from memory impairment, I recommend that you do not delay contacting a specialist.
Classification
The modern classification of cognitive disorders is based on the degree of their severity and is divided into mild, moderate and severe forms. In mild disorders, processes such as the ability to quickly process incoming information and switching from one type of activity to another are affected. In moderate disorders, memory impairment predominates, which over time can develop into Alzheimer's disease. Severe disorders include disorientation in time, speech suffers, the ability to reproduce words is impaired, and the psyche suffers.
Cognitive brain functions - what is it?
Cognitive (cognitive) functions are the most complex processes occurring in the brain. They provide a rational perception of the surrounding reality, an understanding of the events occurring around a person. Through the cognitive abilities of the brain, people find connections between themselves and what they encounter in everyday life.
Cognitive activity consists of the following functions:
- Memory . This term refers to the special ability of the brain to assimilate incoming information, store it and, if necessary, reproduce it.
- Gnosis . This function is responsible for the perception of incoming information from the outside world. Gnosis refers to the brain’s ability to process data and synthesize the simplest sensations coming from all senses into holistic structures.
- Speech . This concept refers to a person’s ability to exchange previously acquired information through statements.
- Praxis . This term refers to a person's ability to acquire and retain new motor skills and then use them in everyday life.
- Intelligence . It refers to the ability to compare incoming information, find commonalities and differences. A person’s ability to make judgments and draw various conclusions on a particular issue depends on the level of intelligence.
Problems with memory and intelligence occur when any part of the brain is damaged. Violations of other cognitive functions occur when certain parts of the central nervous system are damaged (parietal, frontal, temporal and other lobes).
Prevention
What should you do to avoid cognitive impairment? From a young age you need to take care of your health. To prevent this problem, doctors recommend engaging in active sports every day, training your memory, and communicating more. A huge role is played by giving up bad habits, sufficient intake of vitamins, and proper nutrition. For example, a Mediterranean diet can help reduce the risk of developing disorders. Recently, herbal remedies from ginkgo biloba have been used for prevention.
Cognitive disorder in children
The development of cognitive functions mostly depends on the supply of vitamins and other useful substances to the human body.
Today, unfortunately, the problem of hypovitaminosis in children is becoming quite acute. The consumption of refined food products, shelf-stable products, and goods that have been subjected to prolonged temperature treatment makes it impossible to replenish the required amount of essential micronutrients through diet alone.
According to studies conducted in recent years on the vitamin and mineral state of children's bodies, it can be concluded that the lack of ascorbic acid (vitamin C) among the country's child population reaches almost 95%, approximately 80% of children have a deficiency of thiamine (vitamin B1), riboflavin (vitamin B2 ), pyridoxine (vitamin B6), niacin (vitamin B4 or PP) and folic acid (vitamin B9). Cognitive functions are a complex phenomenon that is not fully understood today. However, a whole range of studies conducted assessing individual cognitive processes, for example, such as reproduction, memory, clarity of mental perception, intensity of thought processes, ability to concentrate, learning, problem solving, mobilization, made it possible to trace a clear relationship between the cognitive functions of children and their provision of certain micronutrients .
Today, cognitive impairment is one of the most important problems in psychiatry and neurology. Such pathologies, unfortunately, are observed in approximately 20% of children and adolescents.
The prevalence of speech and language disorders, which include writing and reading disorders, ranges from 5% to 20%. Autism spectrum disorders reach almost 17%. Lack of attention combined with increased activity is observed in approximately 7% of individuals in childhood and adolescence. Disorders of psychological development, emotional disorders, mental retardation syndromes and behavioral disorders are also widespread. However, most often one can note the occurrence of a disorder in the development of learning skills, motor processes, and mixed specific developmental disorders.
Cognitive disorders in children most often occur due to diseases characterized by dysgenesis of the cerebral cortex, congenital metabolic disorders affecting the nervous system, degenerative diseases, and damage to the nervous system during the period of fetal formation.
Damages to the nervous system in the perinatal period include: brain hypoxia, trauma received during childbirth, intrauterine infection. Therefore, to this day, the diagnosis of the initial phases of cognitive function disorders in children remains an important problem. Its early results will contribute to more timely prescription of appropriate therapy and the prevention of early disability in children. Today, the diagnosis of childhood pathologies in the cognitive sphere is possible only with the help of a comprehensive clinical examination, clinical-psychopathological examination, psychometric, and neuropsychological research methods.
Beck Depression Scale (test questionnaire). Beck's cognitive therapy or how to get out of depression.
Method The Beck Depression Inventory is used to diagnose the level of depression.
The Beck Depression Inventory was proposed by Aaron T. Beck in 1961 based on clinical observations that revealed a list of symptoms of depression.
After comparing this list with clinical descriptions of depression, a depression questionnaire was created that included 21 statement questions about the most frequently encountered symptoms and complaints.
Each questionnaire item consists of 4-5 statements corresponding to specific manifestations/symptoms of depression. These statements are ranked according to the increasing proportion of the symptom in the overall severity of depression.
Beck Depression Inventory (Scale):
The following is Cognitive Therapy, created by Aaron Beck, in which he describes the causes, symptoms of depression and possible ways to get rid of it.
Instructions.
This questionnaire contains groups of statements. Read each group of statements carefully. Then identify one statement in each group that best matches how you felt THIS WEEK AND TODAY. Check the box next to the statement you selected. If several statements from one group seem equally good to you, then check the box next to each of them. Before making your choice, make sure you read all the statements in each group.
Stimulus material.
1 0 I don't feel upset or sad. 1 I'm upset. 2 I'm upset all the time and can't turn it off. 3 I'm so upset and unhappy that I can't stand it. 2 0 I'm not worried about my future. 1 I feel confused about the future. 2 I feel like there is nothing in the future for me. 3 My future is hopeless and nothing can change for the better. 3 0 I don't feel like a failure. 1 I feel that I have failed more than other people. 2 When I look back at my life, I see many failures in it. 3 I feel that as a person I am a complete failure. 4 0 I get as much satisfaction from life as before. 1 I don't get as much satisfaction from life as I used to. 2 I no longer get satisfaction from anything. 3 I'm completely dissatisfied with life and I'm tired of everything. 5 0 I don't feel guilty about anything. 1 Quite often I feel guilty. 2 Most of the time I feel guilty. 3 I constantly feel guilty. 6 0 I don't feel like I can be punished for anything. 1 I feel like I might be punished. 2 I expect that I might be punished. 3 I feel already punished. 7 0 I am not disappointed in myself. 1 I was disappointed in myself. 2 I'm disgusted with myself. 3 I hate myself. 8 0 I know that I am no worse than others. 1 I criticize myself for mistakes and weaknesses. 2 I blame myself all the time for my actions. 3 I blame myself for everything bad that happens. 9 0 I have never thought of committing suicide. 1 Thoughts of committing suicide come to me, but I will not carry them out. 2 I would like to commit suicide. 3 I would kill myself if the opportunity presented itself. 10 0 I don't cry more than usual. 1 I cry more often now than before. 2 Now I cry all the time. 3 I used to be able to cry, but now I can’t, even if I want to. 11 0 Now I'm no more irritable than usual. 1 I get irritated more easily than before. 2 Now I constantly feel irritated. 3 I became indifferent to things that used to irritate me. 12 0 I have not lost interest in other people. 1 I am less interested in other people than before. 2 I almost lost interest in other people. 3 I have completely lost interest in other people. 13 0 I put off making a decision sometimes, just like before. 1 I put off making decisions more often than before. 2 I find it harder to make decisions than before. 3 I can't make decisions anymore. 14 0 I don't feel like I look any worse than usual. 1 I worry that I look old and unattractive. 2 I know that there have been significant changes in my appearance that make me unattractive. 3 I know I look ugly. 15 0 I can work as well as before. 1 I need to make an extra effort to start doing something. 2 I have difficulty forcing myself to do anything. 3 I can't do any work at all. 16 0 I sleep as well as before. 1 I sleep worse now than before. 2 I wake up 1-2 hours earlier and find it difficult to fall back to sleep. 3 I wake up several hours earlier than usual and can’t go back to sleep. 17 0 I'm no more tired than usual. 1 Now I get tired faster than before. 2 I get tired of almost everything I do. 3 I can't do anything because I'm tired. 18 0 My appetite is no worse than usual. 1 My appetite is worse than before. 2 My appetite is much worse now. 3 I have no appetite at all. 19 0 I have not lost weight recently or have only had little weight loss. 1 Recently I have lost more than 2 kg. 2 I lost more than 5 kg. 3 I lost more than 7 kr. I intentionally try to lose weight and eat less (check with a cross). Yes_________ No_________ 20 0 I am no more worried about my health than usual. 1 I am worried about my physical health problems, such as pain, upset stomach, constipation, etc. 2 I am very worried about my physical condition and find it difficult to think about anything else. 3 I'm so worried about my physical condition that I can't think about anything else. 21 0 I haven't noticed a change in my interest in intimacy lately. 1 I am less concerned with intimacy issues than before. 2 Now I am much less interested in intersexual relations than before. 3 I have completely lost libido interest.
Processing the results.
The score for each category is calculated as follows: each item on the scale is scored from 0 to 3 according to the increasing severity of the symptom.
The total score ranges from 0 to 62 and decreases as the condition improves.
Interpretation (key) of the Beck test.
The test results are interpreted as follows:
- 0-9 - no depressive symptoms
- 10-15 - mild depression (subdepression)
- 16-19 - moderate depression
- 20-29 - severe depression (moderate)
- 30-63 - severe depression
The method also distinguishes two subscales:
- Items 1-13 - cognitive-affective subscale (CA)
- Items 14-21 - subscale of somatic manifestations of depression (SP)
Beck's cognitive therapy. How to get out of depression.
Aaron Beck expresses a fundamentally new approach to the correction of emotional disorders, different from the traditional schools of psychoanalysis and behavioral therapy.
The definition of cognition is the psychological process by which information is processed by our consciousness.
A cognitive approach to emotional disorders, aka depression, changes a person's view of himself and his problems. It is necessary to learn to see in yourself an individual who is prone to giving rise to erroneous ideas, but also capable of abandoning erroneous ideas or correcting them. Only by identifying or correcting thinking errors can a person create for himself a life with a higher level of self-actualization.
The main idea of cognitive psychocorrection by A. Beck is that the decisive factor for the survival of the organism is the processing of information. As a result, behavioral programs are born. A person survives by receiving information from the environment, synthesizing it and planning actions based on this synthesis, i.e. developing your own behavior program. The program can be normal (adequate) or inadequate. In the case of a cognitive shift in information processing, an anomalous program begins to form.
Personality, according to A. Beck, is formed by schemas or cognitive structures, which represent basic beliefs (worldview). These schemas begin to form in childhood based on personal experiences and identification (comparing and finding similarities) with significant others. Each person forms his own concept of himself (self-image), others, the world and the concept of his existence in the world.
Schemas are stable cognitive structures that become active when exposed to certain stimuli, stress, or circumstances. Schemas can be either adaptive or dysfunctional.
The “cognitive triad of depression” includes:
- negative self-image (“I am unfit, worthless, a rejected loser”);
- negative view of the world (the person is convinced that the world makes excessive demands on him and erects insurmountable barriers to achieving goals and that there is no pleasure or satisfaction in the world);
- a nihilistic, negative view of the future (The person is convinced that the difficulties he is experiencing are insurmountable. Suicidal thoughts can arise from a feeling of complete hopelessness).
Thus, emotional disturbances and behavioral disorders are seen as arising from cognitive structures and as a consequence of actual cognitive processes (in which thought-cognition acts as intermediate variables).
Psychological disorders are associated with aberrations of thinking. By aberration of thinking, A. Beck understood disorders at the cognitive stage of information processing that distort the vision of an object or situation. Distorted cognitions, i.e. Cognitive distortions cause false beliefs and self-signals and, as a result, inadequate emotional reactions.
Cognitive biases are systematic errors in judgment influenced by emotions. These include:
1. Personalization - the tendency to interpret an event in terms of personal meanings. For example, people with increased anxiety believe that many events that are completely unrelated to them concern them personally or are directed against them personally.
2. Dichotomous thinking. In this case, a person tends to think in extremes in situations that touch his sensitive areas, such as self-esteem, with the likelihood of being in danger. An event is designated only in black or white, only as good or bad, beautiful or terrible. This property is called dichotomous thinking. A person perceives the world only in contrasting colors, rejecting halftones and a neutral emotional state.
3. Selective abstraction (extraction). This is the conceptualization (raising into a rule, law) of situations based on details extracted from the general context, while ignoring other information. For example, at a noisy party, a young man begins to be jealous of his girlfriend, who leaned towards another person in order to hear him better.
4. Arbitrary conclusions - conclusions that are unproven or even contradict the obvious facts. For example, a working mother concludes at the end of a hard day: “I am a bad mother.”
5. Overgeneralization is an unjustified generalization based on a single case. For example, a person made a mistake, but thinks: “I always do everything wrong.” Or after an unsuccessful date, a woman concludes: “All men are the same. They will always treat me badly. I will never succeed in relationships with men.”
6. Exaggeration (catastrophization) - exaggeration of the consequences of any events. For example, a person thinks: “If these people think badly of me, it will be simply terrible!”; “If I’m nervous during the exam, I’ll definitely fail and they’ll kick me out right away.”
Stages of cognitive correction work to help get out of depression.
1. Reduction of problems - identification of problems that have the same causes and their grouping. This applies to both symptoms (somatic, psychological, pathopsychological) and emotional problems themselves.
Another option for reducing problems is to identify the first link in the chain, which starts the entire chain of symbols.
2. Awareness and verbalization of maladaptive cognitions that distort the perception of reality.
A maladaptive cognition is any thought that evokes inappropriate or painful emotions and makes it difficult to solve a problem. Maladaptive cognitions are of the nature of “automatic thoughts”: they arise without any preliminary reasoning, reflexively. For a person, they have the character of plausible, well-founded, and beyond doubt. “Automatic thoughts” are involuntary and do not attract a person’s attention, although they direct his actions.
To recognize maladaptive cognitions, the technique of “collecting automatic thoughts” is used.
The person is asked to focus on thoughts or images that cause discomfort in a problematic situation (or similar to it). By focusing on automatic thoughts, he can recognize them and record them.
3. Distancing is a process of objective consideration of thoughts, in which a person views his maladaptive cognitions as psychological phenomena isolated from reality.
After he has learned to identify his maladaptive cognitions, he needs to learn to look at them objectively, i.e. distance yourself from them.
Distancing increases the ability to draw the line between an opinion that needs to be justified (“I believe that ...”) and an irrefutable fact (“I know that ...”). Distancing develops the ability to differentiate between the external world and one’s relationship to it. By substantiating and proving the reality of one’s automatic thoughts, it is easier for a person to distance himself from them, and the skill of seeing hypotheses in them rather than facts is formed. In the process of moving away, the way of distorting the perception of an event becomes clearer to a person.
4. Changing the rules governing the rules of conduct.
To regulate his life and the behavior of other people, a person susceptible to depression uses rules (instructions, formulas). These systems of rules largely determine the designation, interpretation and evaluation of events. Those rules for regulating behavior that are absolute in nature entail regulation of behavior that does not take into account the real situation and therefore creates problems for a person.
In order for a person not to have such problems, he needs to modify them, make them less generalized - generalized, less personalized - related to him personally, more flexible, more taking into account reality.
The content of the rules for regulating behavior is gathered around two main parameters: danger - safety and pain - pleasure.
The hazard-safety axis includes events associated with physical, psychological or psychosocial risk. A well-adapted person has a fairly flexible set of precise rules that allows him to relate them to the situation, interpret and assess the existing degree of risk. For example, a person who is guided by the rule “It will be terrible if I am not at my best” experiences difficulties in communication due to an unclear definition of the concept of “being at my best,” and his assessment of the effectiveness of his interactions with his partner is associated with the same uncertainty. A person projects his assumptions about failure onto others’ perceptions of him, i.e. believes that this is how others perceive him.
All methods of changing rules related to the danger-safety axis come down to restoring a person’s contact with the avoided situation. Such contact can be restored by immersing oneself in the situation in the imagination, at the level of real action with clear verbalization (a clear verbal description) of new rules of regulation, allowing one to experience a moderate level of emotions.
Rules centered around the pain-pleasure axis lead to an exaggerated pursuit of certain goals to the detriment of others. For example, a person who follows the rule “I will never be happy unless I am famous” dooms himself to ignore other areas of his relationships in favor of depending on this rule. After identifying such positions, a person needs to realize the inferiority of such rules, their self-destructive nature. It is necessary to understand that a person would be happier and suffer less if he were guided by more realistic rules.
Classification of behavioral rules:
- 1. Rules that formulate value systems that evoke certain stimuli that are subjectively perceived differently and generate positive or negative emotions in a person (for example: “Unwashed vegetables are carcinogenic”).
- 2. Rules associated with the impact of the stimulus (for example: “After the divorce, everything will be different”).
- 3. Behavioral assessments (for example: “Because I stutter, no one listens to me”).
- 4. Rules related to the emotional and affective experience of the individual (for example: “At the mere memory of the exam, I get a shiver in my back,” “I have no more hope”).
- 5. Rules related to the impact of the reaction (for example: “I will be more punctual so as not to anger the boss”).
- 6. Rules associated with obligation and arising in the process of socialization of the individual (for example: “A person must receive a higher education in order to be happy”).
5. Change of attitude towards the rules of self-regulation.
6. Checking the truth of the rules, replacing them with new, more flexible ones.
Section: psychology tests with answers.
Personality psychology tests.
Beck Depression Scale (test questionnaire). Beck's cognitive therapy or how to get out of depression.
Rate this article:
Rating 4.94 (17 Votes)
More on the topic:
- How to bring back the joy of life?
- Reasons for failure. Or what is needed to achieve your goal? Psychocybernetics.
- Coping strategies. Test Overcoming Difficult Life Situations (PTLS).
- Anonymously ask a psychologist a question and get advice online.
- Paid consultation with a psychologist.
- Back: How to achieve your goal. Possible obstacles and overcoming them. Tests in pictures. Projective techniques.
- Next: Time management. Test-questionnaire for self-organization of activities (OSD). Psychodiagnostics of time management.
Complex of provoking factors
There are more than 10 different factors that can lead to cognitive disorders of brain function. The most common cause of such disorders is Alzheimer's disease. This pathology is accompanied by the gradual death of brain neurons, as a result of which its individual functions are suppressed.
The first and most striking sign of Alzheimer's disease is memory loss. At the same time, motor activity and other cognitive functions remain within normal limits for a long time.
In addition to Alzheimer's disease, a decrease in a person's intellectual capabilities is observed in the following neurodegenerative pathologies:
Quite often, cognitive disorders can manifest themselves in vascular diseases of the brain. These include:
Basically, dementia and other forms of psychoneurological disorders are caused by a combination of vascular pathology and circulatory failure in the brain. The risk group for developing such complications includes people who have been diagnosed with:
- atherosclerosis;
- hypertension;
- arterial hypertension.
Cognitive deficits can also develop with the following diseases (although with much lower risks than in the previous case):
Among the probable causes of the development of psychoneurological disorders are severe poisoning and long-term use of psychotropic substances. Head injuries can also lead to dementia and mild impairment of brain function.
Clinical picture
The intensity of the clinical picture is determined by the severity of the lesion and the location of the pathological process in the brain. In most cases, several types of cognitive disorders of varying severity and intensity are observed.
Neurological diseases manifest themselves in the form of the following phenomena:
With dementia, patients lose the ability to critically assess their own condition, and therefore, when interviewed, they do not complain about the above symptoms.
The first sign indicating a cognitive deficit is memory loss. This symptom occurs even with mild forms of brain dysfunction. At the initial stages, the patient loses the ability to remember information that was received relatively recently. As the pathological process develops, he forgets events that happened in the distant past. In severe cases, the patient is unable to say his own name and identify himself.
Symptoms of disorders with moderate brain damage often go unnoticed. Such disorders are sluggish in nature and do not transform into dementia. The presence of moderate disorders can be determined by the following symptoms:
- difficulties in performing simple counting operations;
- problems repeating recently learned information;
- disruption of orientation in a new area;
- difficulty finding words during a conversation.
A mild form of cognitive impairment is indicated by:
- memory loss;
- problems with concentration;
- high fatigue when performing mental work.
Cognitive impairment must be differentiated from other forms of neurological disorders. In particular, to make a correct diagnosis, it is necessary to establish the presence or absence of pathological changes in a person’s behavior and emotional state.
Prevention and prognosis
A general prognosis for cognitive disorders cannot be made. In each case, the consequences are individual. But provided that you seek help from a specialist in a timely manner and follow all medical instructions, it is possible to stop the development of the pathological process.
It is important to note that there are two types of cognitive impairment: reversible and irreversible. The first form can be corrected, but the second cannot.
Prevention includes measures aimed at reducing stress and increasing a person’s mental and physical activity. To avoid the occurrence of such disorders, it is recommended to regularly perform intellectual tasks from a young age.
In addition, in order to prevent dementia, vascular pathologies and liver diseases should be treated promptly, and the deficiency of B vitamins should be regularly compensated.
Treatment
If a mild developmental cognitive disorder is diagnosed, your doctor may prescribe a vitamin and mineral course. You should consult your doctor about taking any medications, because self-medication is dangerous.
Treatment of diagnosed cognitive disorders and the duration of therapy will be determined depending on the cause of the disorders. The main problem that needs to be solved is the correction of all changes that have occurred in the brain.
Treatment will be carried out as follows:
- therapy of the underlying pathology;
- restoration of disorders in the brain;
- prevention of relapse.
If a patient has cognitive developmental impairment due to schizophrenia, then the person is prescribed certain medications. Dosage and course are determined individually.
Write out:
- drugs against hypercholesterolemia;
- cholesterol-free diet - the patient is recommended to consume more cottage cheese, skim milk, fresh vegetables and fruits, and seafood;
- recommend giving up bad habits;
- Cognitive psychotherapy is carried out for emerging disorders.
If developing cognitive disorder is diagnosed in children, treatment is always carried out in combination:
- drug therapy mainly uses nootropic drugs that restore metabolic processes and improve interneuron transmission - this has a positive effect on mental abilities, concentration, speech and learning.
- non-drug treatment, which includes sessions with a psychotherapist.
The patient must constantly train his memory, for example, he can learn lyrics or poems.
How to improve the patient's condition?
When selecting a treatment regimen for a patient, it is important to first establish the cause of the development of cognitive disorder. Therefore, after assessing the mental status, a comprehensive examination of the patient is carried out.
Treatment tactics for disorders are determined based on the severity of the disease and the cause of the brain dysfunction. In the treatment of mild to moderate dementia caused by Alzheimer's disease or vascular pathologies, acetylcholinesterase inhibitors or Memantine are used. However, the effectiveness of these drugs has not yet been proven. They are prescribed mainly to prevent further progression of the pathological process and the development of dementia.
In case of diagnosing vascular pathologies that provoke a failure of brain activity, the following are used:
- phosphodiesterase inhibitors promote vasodilation, which leads to normalization of blood circulation;
- α2-adrenergic receptor blockers suppress the actions of the sympathetic nervous system, which lead to the narrowing of blood vessels.
Actovegin is used to restore neurometabolic processes. The drug increases the plasticity of brain neurons, which has a positive effect on cognitive functions.
In addition to these medications, in the presence of neurological disorders, various therapeutic tactics are used to correct the patient’s behavior. It takes a lot of time to complete this task, since such treatment involves a consistent transformation of the human psyche.
Tactics for managing a patient with impaired cognitive functions: