Vascular dementia is a group of pathologies characterized by the development of symptoms of dementia and associated with damage to brain tissue as a result of a disorder in their blood supply. This type of dementia is one of the most common. The disease greatly affects the patient's intellectual abilities and his adaptation in society.
Causes
Dementia of the vascular type develops as a result of the death of brain cells caused by a circulatory disorder (lack of or complete stoppage) in any part of it. Disruption of blood flow to brain tissue can occur acutely or be chronic.
Acute circulatory disorder
Acute vascular dementia develops with ischemic or hemorrhagic stroke. Ischemic stroke can be triggered by pathologies such as atherosclerosis, some heart diseases and cerebral vascular abnormalities. In this case, the cerebral arteries are blocked by a thrombus or embolus, which impedes blood flow.
Hemorrhagic stroke is accompanied by hemorrhage that occurs when pressure increases and pathologies of the walls of brain vessels (due to atherosclerosis, intoxication or inflammation). Blood pours into the brain tissue by breaking the integrity of the vessel or “leaks” through the wall of the affected artery.
Both types of stroke are acute, with pronounced symptoms and lead to the immediate death of a large number of brain cells, which entails the development of dementia. The severity of the disorders depends on the location and size of the lesion.
Chronic circulatory pathologies
Chronic circulatory disorders are not accompanied by pronounced manifestations. In this case, brain neurons die gradually due to impaired blood flow in small vessels (with atherosclerosis) or poor circulation, characteristic of cardiovascular failure. Due to compensation mechanisms for such pathologies, vascular dementia in the initial stages goes unnoticed for a long time by the patient and his loved ones.
At-risk groups
Patients with pathologies such as diabetes mellitus, arterial hypertension, vascular diseases of the brain, heart and peripheral circulatory system have a higher risk of developing vascular dementia. The greatest likelihood of being affected by the disease was found in people over 60 years of age and smoking patients. It is also known that men suffer from vascular dementia much more often.
Symptoms
The initial stages of the development of this disease in older people are asymptomatic in most cases. The time at which the first clinical signs appear will depend on the etiological factor. Thus, with a stroke, the first symptoms in older people appear after 1-3 months. In the event that dementia of the Alzheimer's type manifests itself against the background of several microstrokes and other etiological factors, then pronounced symptoms can be observed six months later.
In general, the clinical picture is characterized as follows:
- gradual memory deterioration. It should be noted that, unlike Alzheimer's disease, in this case this process occurs in a milder form;
- slowing down of mental activity;
- changes in a person’s psychotype;
- narrowing the range of interests. To some things that previously interested the patient, he shows complete indifference;
- periods of apathetic mood;
- speech and writing disorders;
- it becomes difficult for the patient to perceive new information and even individual words;
- excessive talkativeness with a lack of understanding of the essence of what was said;
- the patient does not understand the speech addressed to him if it consists of several sentences;
- long-term memory deteriorates - some life events are completely erased;
- social maladaptation - a person cannot make a purchase on his own, pay for transport fare, gets lost in the area;
- changes in gait are observed;
- The simplest everyday operations are also beyond the power of a person;
- attacks of depression and psychosis;
- epileptic seizures.
In the final stages of the development of the disease, a person is no longer able to perform simple actions of self-care and to cope with natural physiological needs. At this stage of development of the disease, the patient needs round-the-clock care; he cannot be left alone, as this is dangerous for his life and for those around him.
Despite the fact that the clinical picture of senile dementia of this form is clearly expressed, in no case should you independently compare symptoms and treatment and carry out therapeutic measures on this basis.
Classification
Vascular dementia is classified according to two criteria: the etiology (cause) of the disease and the location of the lesion in the brain. This pathology also has its own code in the International Classification of Diseases, 10th revision (ICD-10).
ICD-10
The ICD-10 code for vascular dementia is F01. Vascular dementia in this classification is defined as the result of cerebral infarction due to pathology of its blood vessels. This section includes several subtypes of vascular dementia:
- Vascular dementia with acute onset (F0). This pathology occurs after several cerebral strokes that developed due to thrombosis of cerebral vessels, embolism or hemorrhage. Also, the cause of this type of dementia can be a single extensive cerebral infarction.
- Multi-infarct dementia (F1). It is characterized by a smooth course with repeated transient ischemic phenomena, as a result of which an increase in infarct zones in the brain substance occurs. The cerebral cortex is predominantly affected.
- Subcortical vascular dementia (F2). This includes clinical situations when the medical history of vascular dementia contains a history of hypertension and ischemic foci of destruction located in the white medulla. The cortical substance is preserved, which makes it possible to distinguish the clinical manifestations of this pathology from Alzheimer's disease.
- Mixed cortical and subcortical vascular dementia (F3).
- Other vascular dementia (F8).
- Vascular dementia, unspecified (9).
This classification allows you to assign a specific code to the disease, which will be understandable to specialists around the world.
Classification according to etiology and localization of the lesion
For the reason that led to the development of pathology, the following varieties are distinguished in vascular dementia:
- dementia caused by a brain stroke;
- dementia due to chronic ischemia;
- mixed vascular dementia, including various causative factors.
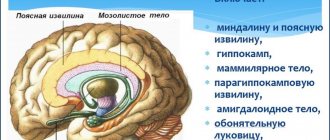
Vascular dementia is classified according to the location of the affected area:
- subcortical;
- temporal region;
- frontal lobe;
- midbrain;
- cerebral cortex;
- mixed cortical and subcortical.
The symptoms of the pathology directly depend on the cause of dementia and the location of the lesion.
Mechanism of disease development
Acute disturbances in cerebral blood flow or chronic insufficiency of blood supply to the brain lead to the fact that some neurons stop receiving oxygen and nutrients. This causes cell death.
If the lesion leads to infarction of a small number of neurons, then other brain cells are able to compensate for the loss. In such cases, only damage to a large area of the brain leads to the development of symptoms of vascular dementia. However, if neurons that perform cognitive functions are affected, then the death of even a small group provokes the onset of dementia.
Clinical manifestations
The main difference between vascular dementia and other types of dementia is the combination of cognitive and neurological impairment.
The nature and severity of the disorders depend on the location and size of the lesion. Comparison of vascular dementia with Alzheimer's disease
| Sign | Alzheimer's disease | Vascular dementia |
| Onset of the disease | Always smooth and unnoticeable, after 40 years (more often in people over 65 years old). | May be acute or gradual and unnoticeable. They can appear at any age, but more often in people over 65 years of age. |
| The presence of this pathology in any relatives | Sometimes | Rarely |
| Main cognitive symptom | Memory disorder | Impaired ability to plan and control |
| Neurological disorders | No | Varied |
| Changes on MRI | Atrophy of the cerebral cortex and hippocampus (not always) |
|
The most typical manifestations of this type of dementia are: inhibition of mental reactions, decreased mental flexibility, narrowing and limitation of the patient’s range of interests.
Main symptoms
The disease vascular dementia has a whole complex of symptoms, the presence and severity of which depends on the location of the lesion and the stage of the pathological process. The most common manifestations are:
- frequent depression;
- apathy;
- speech disorders (it becomes slurred);
- memory impairment;
- epileptic seizures;
- inhibition of reactions;
- decreased coordination of movements;
- problems with communication and social perception;
- changes in the emotional sphere;
- inhibition of mental activity;
- disorientation in time and space;
- difficulties with perception and assimilation of information.
Each stage of this type of dementia has specific symptoms.
Stages of the disease
There are three stages of vascular type dementia. Each transition of pathology to a new stage is characterized by the inclusion of new symptoms in the clinical picture and an increase in the severity of existing ones.
initial stage
Cerebrovascular dementia begins with mild symptoms; this is not always noticeable. Usually, the first thing that occurs is memory disorders in the form of episodic forgetfulness and absent-mindedness, which later turns into fixation amnesia. As a result, the person cannot remember recently occurring events or conversations.
Also, this stage of dementia is characterized by an exacerbation of certain character traits. The ability to plan and perform any tasks decreases. It becomes difficult for a person to perform work that requires intellectual activity. The patient forgets some words, his speech is replete with repetitions and filler words.
The patient is prone to anxiety and depression for no particular reason and becomes withdrawn. However, he needs the support of loved ones.
The acute onset of vascular dementia is characterized by the occurrence of epileptic seizures. Also, for a similar course of the disease, impairment of long-term and short-term memory is typical.
Middle stage
As the disease progresses, the memory disorder progresses more and more. Some memories may even be replaced by non-existent ones, however, senile vascular dementia retains the events of childhood and adolescence in memory very vividly and accurately, even in comparison with a healthy person. This stage of dementia is characterized by the phenomenon of pseudoreminescence, in which the patient perceives long-ago events as having happened just a short time ago.
The middle stage greatly impairs the patient's coordination and orientation in space. Because of this, the patient constantly needs accompaniment on the street and help with household chores. The patient's interests are narrowed and limited, for example, to only watching TV series.
Severe stage
Severe vascular dementia is characterized by an increase in all symptoms. The patient practically does not speak, the reaction to external stimuli is low, and attacks of aggression are also possible. Gradually, there is a degradation of all functions of the body, starting from the fading of motor abilities to changes in the mental state and loss of personality.
Vascular dementia: causes, clinical picture
Depending on the location of the lesion, dementia is divided into categories. Different parts of the brain are responsible for different human actions and skills. It is often possible to use these lost skills to diagnose which part of the brain is affected and how deeply. Cortical, subcortical and mixed vascular dementia are diagnosed based on the patient's symptoms.
Cortical dementia is characterized by memory problems and loss of cognitive function. Speech and orientation in space are impaired, logic, recognition (gnosis) and automatism (praxis) are lost.
The patient may forget his loved ones and get lost in his room. Praxis is an automatic action that a healthy person performs without thinking about it. We eat soup with a spoon, but we don’t think about how it happens. The hand and mouth themselves act according to an established pattern, but with the loss of praxis this automatism disappears.
With subcortical dementia, forgetfulness and some slowness in movements and walking appear. Also an indispensable companion to subcortical dementia is apathy or depression.
The temporal region of the brain (hippocampus) affects human memory. If this part of the brain is damaged, memory loss or complete loss is noted. First, short-term memory is lost, and the patient may forget what he did a minute ago. A little later, the patient begins to remember events that happened a long time ago, even in distant childhood. Moreover, these memories are very clear, precise and detailed.
The frontal lobes of the brain are adequacy and psycho-emotionality. Disturbances in the blood supply to this part of the brain manifest themselves in various types of behavioral abnormalities. Obsession with words, actions, inability to trace cause-and-effect relationships, all this indicates a disruption in the functioning of the frontal lobes of the brain.
The subcortex of the brain is memorization, concentration and logic. Thanks to the correct functioning of the subcortex, we count, write and are able to focus on a specific task. If dementia affects the subcortex, then these skills are lost.
If only one part of the brain is affected by injuries, and the disease can be localized, then with dementia caused by vascular atrophy, strokes, Alzheimer's disease, the disease is difficult to stop, because the death of neurons is a consequence, the reasons lie elsewhere.
The diagnosis of vascular dementia has many classifications. If previously dementia was considered a disease of old age, now everyone is at risk.
✔️ Atrophic dementia (Alzheimer's type) - occurs due to the gradual death of brain neurons.
This type of dementia appears due to a disruption in the blood supply to brain cells, and neurons die precisely because of oxygen starvation. Cerebral ischemia can provoke dementia. This is a blockage of small vessels and blood does not flow properly to the brain.
✔️ Mixed vascular dementia is a disease that combines vascular and atrophic dementia at once.
✔️ Among the causes of senile (senile) dementia is an incorrect lifestyle in youth, i.e. alcohol abuse, smoking, addiction to psychotropics, overeating and low activity. In youth, the body more or less copes, but closer to old age, the blood vessels are already too weak, which leads to brain starvation and the death of brain cells.
Dementia is getting younger, and now its victims are people who have barely crossed the 50-year mark. This disease is hereditary, and even if you lead a healthy and correct lifestyle, if you have a history of close relatives with dementia, you can easily join the ranks of those affected.
Diagnostics
The diagnosis of vascular dementia in older and younger people is established on the basis of anamnesis, the presence of characteristic symptoms in the patient and the results of various studies.
Important! A complete and timely diagnosis will help identify pathological changes in the early stages, which will allow treatment to be carried out much more effectively!
To determine the disease that caused the development of dementia, the patient is referred for examination to various specialists (neurologist, cardiologist, psychiatrist, etc.).
Blood pressure is also monitored, since hypertension is one of the most common factors in the development of vascular dementia. Localization of brain lesions in various types of dementia
| Localization of the lesion | Relevant diagnoses |
| Cerebral cortex |
|
| Subcortical zone |
|
| Cortical-subcortical |
|
Computed tomography of the head, Doppler ultrasound of cerebral vessels, electrocardiography, as well as MRI for vascular dementia will help determine the presence, nature and localization of pathologies that led to the onset of dementia.
Diagnostic measures
With timely diagnosis of vascular dementia, a complete recovery of the patient is possible. In other cases, a correct diagnosis can reduce the rate of development of pathology. For this purpose, the following diagnostic measures are used in modern neurology:
- Examination of the patient, careful collection of medical history;
- Psychological testing to determine the presence and severity of disorders;
- Pressure monitoring;
- Determination of glucose and cholesterol in the bloodstream to determine the presence of diabetes mellitus and atherosclerosis;
- Radioisotope research;
- Carrying out magnetic resonance or computed tomography. The techniques allow us to determine the degree of damage to brain tissue;
- Dopplerography of cerebral vessels allows you to study blood flow in the brain;
- Angiography is radiography of brain vessels.
An accurate diagnosis can only be made on the basis of a comprehensive diagnosis and comparison of the results obtained.
Treatment
Therapy for vascular dementia is carried out based on the nature and course of the underlying disease. The main goal of treatment is the maximum restoration and preservation of adequate blood circulation in the brain and compensation for disorders that appear against the background of vascular pathology.
Important! A healthy lifestyle is one of the main aspects of disease prevention!
Clinical recommendations for vascular dementia include specific diet and physical activity. Drug therapy usually consists of the following:
- nootropic drugs;
- antioxidants;
- vasoactive medications;
- neuropeptides;
- MAO enzyme inhibitors;
- neurotrophic drugs;
- drugs that stabilize neuron membranes, etc.
For increased anxiety and sleep disturbances such as insomnia, sedatives are prescribed, and if the disease leads to dangerous mental problems, antipsychotics are used. Depression that occurs with vascular dementia can be successfully treated with serotonin reuptake inhibitors.
Drug treatment is not complete. Therapy for vascular dementia should include other techniques (physical treatment, psychotherapy sessions, etc.). Proper patient care also plays an important role, on which the patient’s condition directly depends.
Stages of vascular dementia
Vascular dementia in medical reference books has a code according to ICD 10, with typology F00-F09. According to the description, vascular dementia is characterized as dementia, organic dysfunction, memory disorder, behavior and thinking. With the disease, not only intellectual abilities suffer, but also personality is destroyed.
Senile dementia is poorly understood, but in some cases it is believed to be caused by Alzheimer's disease. In such cases, the disease progresses rather slowly, silently affecting various parts of the brain.
Secondary vascular dementia occurs against the background of damage to certain areas of the brain due to injury, stroke or atherosclerosis. With timely and adequate treatment, some functions can be restored and the course of the disease can be slightly slowed down. With proper rehabilitation, certain cognitive functions can be restored, and the patient will be able to care for himself independently. Secondary dementia is partially reversible if proper efforts are made to restore it.
Dementia often results from infectious diseases of brain neurons, tumors and other degenerative brain diseases. Syphilis and meningococcal infections can cause dementia. Such cases are about 5-10%, but they do happen.
Unidentified causes of dementia are designated by code F03, with an explanation of the possible causes of the disease (see the complete list of mental illnesses). Alcoholism, psychosis, depression, each individual case of illness is assigned its own code.
There are three stages of onset of vascular dementia.
1st degree – a risk factor occurs. These are traumatic brain injuries, heart attacks, strokes, diabetes, varicose veins, tumor diseases of the brain, increased cholesterol, and much more. All these pathologies can trigger the disease.
2nd degree – memory disorder, with confabulations. Lost memory fragments are replaced by fictitious ones, grouchiness or social isolation appears. At this stage, the patient may have difficulty performing daily tasks and self-care.
3rd degree - in some cases, the patient loses a sense of shame and morality, and also does not evaluate his actions. In complex cases, loss of motor activity with simultaneous destruction of personality.
Vascular dementia progresses to the terminal stage quite quickly, and at this stage treatment comes down to patient care. Very quickly all parts of the brain stop functioning, and the patient becomes absolutely helpless. In some diseases, only six months can pass from the onset of the first symptoms to the terminal stage, and there is no way to slow down the course of the disease due to its rapid development.
Signs of the disease
There are three stages of vascular dementia, which are generally characterized by the accumulation of symptoms of dysfunction of the nervous system.
- The mild stage is expressed by such signs as forgetfulness, rapid mood swings, unusual for this person, and inability to concentrate. At this stage, the patients themselves and their relatives attribute such cases to fatigue, stress and old age.
- Moderate vascular dementia is characterized by noticeable symptoms. The person forgets the names of relatives and does not remember recent events, unlike situations that happened many years ago. He might get lost in his own home. Some patients become aggressive or, on the contrary, apathetic. There is a loss of self-service skills: using household appliances, cooking. Cognitive symptoms may be accompanied by neurological ones: gait disturbance, speech problems.
- At the late stage of vascular dementia, the patient is completely dependent on relatives or staff of specialized institutions due to disability. He does not recognize family and friends, loses orientation in space and time. A person needs outside care, including preparing food, feeding, and performing hygiene procedures. Patients often experience involuntary urination.
Without treatment, dementia can progress rapidly due to the development of cerebrovascular insufficiency. Stabilization of cerebral blood flow in the early stages often leads to a significant slowdown in negative dynamics and even to the complete return of lost intellectual functions.
Other risk factors
As a result of long-term research into the causes of dementia, scientists have identified a whole list of factors predisposing to dementia.
- Age over 60 years - about 90% of cases of the disease were recorded in this age category.
It is wrong to think that dementia is a disease exclusively of older people. Among its victims are adults half the age of 60, whose cognitive functions are impaired as a result of traumatic brain injuries and long-term alcohol abuse.
- Chronic increase or decrease in blood pressure leads to strokes, and they, in turn, lead to vascular dementia.
- Diabetes mellitus - diabetics are predisposed to vascular pathologies, what the risk is - see above.
- Bad habits - smoking and drinking alcohol in excessive quantities are a direct path to cardiovascular diseases, and, therefore, to an increased risk of mental disorders.
- Lack of physical activity - a study conducted by American scientists over a quarter of a century showed that out of 19 thousand observed, dementia of vascular origin developed in those who were in poor physical shape.
- Estrogen imbalance – an excessive increase or decrease in the level of the hormone in the blood of women after menopause increases the risk of cognitive disorders. Scientists have not yet given an exact answer to the question of why this happens.
- Male gender – men develop dementia one and a half times more often than women.