Psychiatry is a special field of medicine that studies changes in brain activity that cause mental disorders. Mental illnesses arise as a result of brain damage due to injuries and various diseases - syphilis, schizophrenia, tumor processes, senile changes and others.
Patients do not always understand when to see a psychiatrist and when to see a psychologist or psychotherapist. Psychiatry, psychotherapy and psychology are related disciplines; very often, for the same problems, you can be seen by, for example, a psychiatrist, a psychotherapist, and even a psychologist. If you still try to draw a line, it will be the severity of a person’s psychological problems.
A psychiatrist treats the most severe injuries associated with somatic changes; as a rule, he treats them with medication. A psychotherapist treats less serious illnesses (phobias, neuroses) and focuses on non-drug methods, although he may and has the right to prescribe medications. A psychologist is not a doctor and treats everyday human disorders (problems of personal growth, misunderstanding in the family) exclusively through consultations.
“Am I crazy, or what?”
— Many of us do not like to go to any doctors, and even a visit to a psychiatrist is perceived as something prohibitive. Why? What stops people? After all, sometimes you can’t do without help.
— Firstly, people have little idea what psychiatric disorders are. Most consider only the most severe conditions or those “pictures” that they see in movies and TV series, or read about in books, as disorders. In fact, 80% of what we see in movies for the mass audience is a very approximate variation on the theme of psychiatry,
It is impossible to focus on what patients with mental diagnoses look like in art.
Second. Psychiatry has a bad reputation in Russia. We regularly get stories in the press about how someone was forcibly and harshly, in violation of their rights, “taken to a mental hospital.” Since many of them are true, I do not think that psychiatry should be written any differently. But these publications are unlikely to make the reader go to a neuropsychiatric dispensary with joyful hope.
In addition, our people really do not like to communicate with repressive authorities. And in the history of our country there is recent documented experience of how psychiatry was used to combat undesirables. The myth “I went to the PND and ended up in the KGB” is alive.
Therefore, people are more willing to turn to private psychiatrists or regular (somatic) hospitals. But in fact, the likelihood that you will be tied up and taken somewhere because you woke up in the morning and decided that life has been somehow hard for you for a year now, and you finally need to go to the doctor is practically zero.
There are also people who are contemptuous of everything with the prefix “psycho-”. Many of them cannot distinguish a psychologist from a psychotherapist, but at the same time they are wildly afraid of even the very idea of seeing a specialist: “Am I crazy, or what?” People do not understand that from a psychologist to a psychiatrist is a huge path that they may never travel.
It is also important to understand that the treatment of mental illness is a long story. Often, upon hearing a doctor’s order: “Come back in a week,” patients turn around and don’t come back; I once did that myself. But if, for example, you had surgery on your finger, you will go through all the dressings until your drainage is removed and the wound heals.
It’s the same with a mental diagnosis - it cannot be correctly stated at one time, it can be specified, especially since many mental illnesses have common symptoms.
The most common diseases that require specialist intervention
One particular problem is depression, which can be caused by various reasons. This is not just a bad mood, but a disease, and quite serious, and having clinical manifestations. Most often it appears seasonally.
Main symptoms: sadness, depression, depression, loss of interest in everything, decreased energy, leading to high fatigue and less activity. This also includes low self-esteem, constant self-flagellation, and any actions that are associated with self-deprecation. Often, libido decreases and appetite is disrupted. Excessive fussiness or, conversely, lethargy is possible.
Typically, depressive conditions worsen in the morning, and improve in the evening. If they continue for more than two weeks in a row, then this is already a disease.
Apathy is a complete lack of interest in something. Sometimes it can get to the point where a person stops looking after himself and can die of hunger, lying on the couch at home.
Common problems also include stress, which often occurs due to hard work or constant fatigue.
The patient has the right to any questions
Photo: RIA Novosti
— What needs to be done to get the maximum possible benefit from a visit to a psychiatrist, and not face harm from the shortcomings of our mental health care system?
— The main thing that you must understand is that you have the right to ask a lot of questions: what’s wrong with me, why did you prescribe this, how do these pills affect?
Often a person has a fear of “not liking the doctor” and asking too much. Now such sentiments must be replaced by the confidence that you have the rights of a patient and the opportunity to participate in the treatment of your illness.
From the side of specialists, for me, a sign of an unsafe visit to a psychiatrist was that an unfamiliar doctor immediately prescribed a battery of medications.
If we are talking about a serious illness such as psychosis or another dangerous condition for a person and others, he just needs to be persuaded to go to the hospital. I’m talking about a range of diagnoses from the field of “minor psychiatry” - depression, anxiety-panic disorders.
The fact is that many drugs used in psychiatry have very serious side effects. They affect hormonal levels, metabolism, and heart function; From some pills, very thin people can gain twenty kilograms in a couple of months. Therefore, if pills can be used situationally rather than constantly, or psychotherapy can be used instead of some pills, this should be done.
By the way, you should be very suspicious of a doctor who, having prescribed pills, does not ask you to come back in a week to correct the treatment regimen.
Tablets are not taken immediately, and they should not worsen the condition.
If you sleep all the time, you have a loss of energy, or your head feels as if you are drunk, and this continues for more than a week and a half, during which the body adapts to the drug, the tablets need to be changed.
Pills that work well and are compatible with your metabolism should return you to a state of normalcy, not dullness, but such a drug can rarely be found right away.
The job of a psychiatrist is precisely to listen to your complaints and select a treatment regimen for you.
Another unpleasant moment that makes you doubt the qualifications of a specialist is the imposition of a diagnosis.
That is, if you feel that the doctor is starting to very persistently offer you symptoms (and you are not experiencing them), this is not good. Therefore, before going to the doctor, I would advise you to read about what diseases and conditions there are. Not in order to engage in self-diagnosis - this cannot be done, but in order to understand at the appointment what they are trying to attribute to you.
Often, for example, they try to attribute to you a condition that is worse than yours. According to my observations and that of my friends, this is precisely what IPA doctors suffer from.
I think this is partly dictated by the desire to protect oneself. Because if, for example, a doctor diagnosed a person with a mild degree of depression, and he went and committed suicide, the doctor risks losing his license. And if the patient did something illegal, he could even go to jail.
How to talk to a psychiatrist
Rhythmic photostimulation for brain research in the laboratory of the State Scientific Center for Social and Forensic Psychiatry (SSCSP) named after V.P. Serbian. Photo: RIA Novosti
One of the problems of Russian patients is that they perceive medical institutions as authoritarian. But times change and you need to learn to communicate with a doctor. Yes, he has more diagnostic experience, but only you know what exactly you feel and what your symptoms look like.
When recording, the doctor may exaggerate or minimize them, and you must correct this story.
Remember the principle “Nothing for us without us.”
You can, for example, ask: “Why did you prescribe so many drugs?” And the doctor will answer: “Because you feel bad now.” Or: “You are now experiencing an exacerbation, you need to take a lot of pills for a month, and then we will slowly remove them.”
It is important to ask: “What kind of diagnosis is this, what does it mean? Why are you giving me such recommendations? It is interesting that many patients do not ask for their diagnosis, and for some reason the doctors at the PND do not tell it. But doctors should not hide the diagnosis from the patient. It is illegal.
You can argue with the doctor and ask: “On what basis are you putting this on me? I read about diseases, it seems to me that I don’t have such symptoms, but there are others.”
First appointment with a specialist
This is a very difficult job. At the first visit, the psychiatrist conducts a survey of the patient himself or his relatives if the patient cannot answer truthfully on his own. After testing, a primary diagnosis is established. Then the treatment conditions are determined - inpatient or outpatient. At the end, a treatment strategy is outlined.
An appointment with a psychiatrist is a procedure that you should not be afraid of, since testing and treatment are carried out anonymously and the person is not registered. The survey is carried out only with the written consent of the patient.
What does it mean to be on time?
At the Gerontopsychiatric Mercy Center of the Department of Labor and Social Protection of the Moscow Population. Photo: Alexander Ryumin/TASS
— What should a person do to avoid finding himself in a situation where he gets sick, but cannot understand what’s wrong with him, and ends up getting acquainted with the psycho-help system in the format of involuntary hospitalization?
“At the very least, we have learned that we need to be checked for cancer regularly. Approximately the same needs to be done with psychiatry.
It is important for a person to learn to self-reflect - to periodically think about his feelings, thoughts, state, how he perceives the world and why. After all, a person is responsible for his condition, including his mental one, he can think about prevention, he can read something about psychiatry: then he will notice a sharp loss of strength and a change in emotions, he will realize that this is not like the attacks of sadness that he had him before.
Because an ordinary attack of sadness cannot last a month. The person will notice that it is more difficult for him to interact with people or that he is scared on the subway (panic attacks).
But for this to happen,
The media space should be saturated not only with scary or good stories “from the lives of psychos,” but also with educational information: what are the symptoms of mental illness, how a psychologist differs from a psychiatrist, and so on.
Eventually, people will get used to this information and stop being afraid. Maybe a crowd of healthy people who don’t need to go to the dispensaries will go to the dispensaries, but it’s not scary - the doctors are able to distinguish the sick from the alarmist, and the healthy ones will be sent back.
In my opinion, if you have suspicions, it is better to go to the doctor again. You can start with a psychotherapist; a competent psychotherapist is able to understand whether this is an illness or a life problem.
It would also be a good idea to get checked regularly by a neurologist, because many neurological conditions can be mistaken for psychiatric symptoms.
For example, both psychiatry and neurology can give rise to hallucinations. “The world around me seems blurry” can be derealization and a symptom of very low blood pressure. Cardioneurosis is very similar to a real heart disorder and it is impossible to make this diagnosis without checking the heart.
Fortunately, now many psychiatrists have begun to work in conjunction with neurologists, but in general, isolation is the problem with our system of psychotherapy; the doctor largely relies on the patient’s stories and can confuse the patient’s real condition with what he thinks.
— Find an argument for a person who has problems, but is looking for excuses not to go to a psychiatrist.
“Nothing will happen to you from a single visit to the doctor.” No one will force you to take pills or stay in the hospital. You can always just go to the doctor. If you are worried about the queue at the PND, go to a private one.
You can always stop interacting with the system whenever you want.
You can buy pills and not drink. Drink them twice and stop. This will most likely only make things worse, but such is your will, you are the master of the situation.
You can imagine in advance the worst thing you fear from a visit to a psychiatrist. We have already said that a person who remains critical of his condition is unlikely to be immediately admitted to the hospital. No one will be able to find out about your visit to a doctor - this is personal information, it is protected by law and is given only to the patient himself. If you are afraid of meeting your acquaintances in the IPA queue, go to a private doctor; no one will ever find out from him.
We have not had psychiatric records in its Soviet sense since the 80s of the 20th century. Permanent reports, for which you need to regularly appear in the hospital, now happen either in very difficult cases after forced hospitalization, or by court order if you have done something illegal.
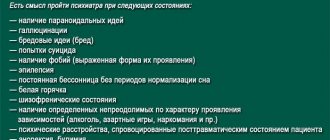
It's time to find a psychotherapist
Sometimes many people have to think about seeing a psychotherapist, how it goes and when to seek help. This becomes relevant when a problem arises that is difficult to cope with on your own. Such problems can be urgent or non-urgent. Among the first are the loss of a loved one, toxic relationships, panic attacks, depression, phobias - everything that makes you feel bad now. Non-urgent ones include cases when a person is constantly coming to terms with something: negativity in his personal life or boring work.
Symptoms that are a reason to make an appointment with a psychotherapist:
- Thoughts about suicide.
- Changes in character: unsociability, loss of interest in business, isolation.
- The desire to harm yourself or marks on the body (cuts, burns, scratches).
- Changes in self-confidence, set-up for failure.
- The appearance or increase in obsessive actions.
- Incomprehensible, strange sensations in the body.
- Panic attacks.
- Irritability and aggression.
- Unexpected emotional reactions: sadness in response to a question about business, tearfulness while watching a comedy.
- Mood swings.
- Unstable appetite.
- Fatigue, drowsiness, apathy.
- Sleep disorders: constant drowsiness, poor sleep quality or insomnia.
- Difficulty concentrating.
- Reluctance to move.
Contraindications to seeing a psychotherapist:
- Children under six years of age.
- Official diagnoses like epilepsy and schizophrenia.
- Lack of desire for changes in life.
- Dementia.
Create a security system
Photo: Alexander Ryumin/TASS
— If the disease is confirmed, does it make sense to tell your family and friends about your situation in order to avoid a situation where you have an exacerbation, but you don’t understand it and can harm yourself?
- Necessarily. Recently, my friend was taken to the hospital as an involuntary admission. Since in these cases the phone is taken away, it is impossible to contact the person, he simply “disappears.”
Similar situations are possible with dementia and with exacerbation of schizophrenia. The strange thing about our system is that in this case relatives will be called only if the person is a minor or has officially registered incapacity. There is a risk that an adult and capable person simply will not be found until discharge.
If a person has a history of psychosis or other serious conditions, one or more people around him should be aware of this. In general, in such a situation, an entire security system should be developed.
For example, for those who have serious conditions, but still have criticism, I strongly do not recommend calling an ambulance for psychiatric help at your home.
It’s better to go to the emergency room with your feet and call an ambulance there. Alas, even if a person called the doctors themselves, there is a risk that he will be taken to the hospital involuntarily and treated rudely, violating his rights.
The functions of the assistant in this case may be different. If something is wrong with a person, and he understands it, an assistant can come, contact the doctor, take him to him and back home, checking that his friend has taken the prescribed pills along the way.
If a person feels bad and he has little control over it, the assistant calls a psychiatric ambulance home, involuntary hospitalization is arranged, but at the same time the assistant makes sure that his friend is treated like a human being, finds out exactly where he was taken, and then regularly calls his doctor and goes to visit the patient.
Try to find out good hospitals in advance and be hospitalized only there. In order to have information about hospitals, you need to be in good contact with doctors, sometimes just with the attending physician from the dispensary.
For example, in the NCPH or Alekseevskaya, the conditions are much better than in the hospital at the regional PND - there are more modern medicines and better living conditions. Unfortunately, people from the regions often have no choice.
In addition, there are cases when hospitalization is not necessary; a person simply needs to relieve an acute condition. For example, he has a severe attack of anxiety or phobia, and he is afraid to go outside, or a hysteria that lasts for several hours. Such conditions are very unhealthy for the brain, they need to be removed, but the patient is not dangerous to himself or others.
In such a situation in Moscow, it is now possible to call for emergency psychiatric help; The team will give you an injection or IV. You need to know about this type of help and, by dialing 103, ask to be transferred to a psychiatric emergency dispatcher or describe the symptoms in detail.
How to reconcile a psychiatrist and a patient: a doctor’s opinion
Victor Lebedev, psychiatrist (Petrozavodsk). Photo: Facebook
Victor Lebedev, psychiatrist (Petrozavodsk)
— In your experience, do our patients dislike only state psychiatry or private ones too?
— There are more complaints about the state one. People are more likely to go to a private owner because they are sure that information from him will not get anywhere. But even to a private psychiatrist (I can say this for sure, since I work in both private and public medicine), patients can throw a tantrum if, for example, he keeps a card for them.
People are so afraid that information about a visit to a psychiatrist will “leak” somewhere that unrealistic demands begin: “You, doctor, examine me, prescribe me pills, but don’t write this down anywhere.”
We have to explain that without an entry in the card there is no examination and treatment. Many patients do not imagine that they will have to return to the doctor, continue or adjust the treatment.
Again I have to explain that the card is being made for me, so that a month later I myself remember what I prescribed for the patient. That sometimes a competent entry in the map can be very much in his interests.
For example, a patient accumulated loans, does not remember this, but before going to the bank he saw a doctor who recorded an exacerbation in him. If the card is properly executed, you can try to terminate the deal through the court.
— Does everyone who comes to you for treatment do it on time?
- It's not always the same. Some come and complain: “I’ve had this condition for a year now.” Usually, on the eve of a visit to the doctor, such patients experience some critical event that still forces them to go to the doctor.
But more and more often, people began to come earlier, without reaching the edge, in a completely productive state, which, once treated, can be changed quite quickly.
People began to pay more attention to themselves. Young people monitor their condition more closely, but they also invited their parents and grandparents to attend.
As a result, we have formed a layer of patients who themselves are involved in the popularization of psychiatry. Such patients read about diagnoses and tell their neighbors: “I went, I felt better, and you should go too.”
And they turn to a psychiatrist not when voices from Mars have been heard for the third week, or they have been taken out of the loop, but when the first signs of trouble appear.
“The doctor has experience of treatment, but the patient has experience of illness”
Psychologist at the Moscow Center for Rehabilitation of Victims of Sexual Aggression while working with a patient. Photo: Anatoly Semekhin/TASS Photo Chronicle
— Are there people who hide their symptoms?
— It all depends on the diagnosis. With delusional disorders, a person cannot tell everything. On the one hand, he does not yet have confidence in the specialist. On the other hand, sometimes he cannot understand what is true around him and what is a manifestation of the disease. And here we need evidence from relatives.
A lot is told at the first appointment. But some traumatic events—like sexual assault—are not easy to share with a stranger and may be something that the person may talk about later.
At the first appointment, I specifically tell patients: “You may not say something, it’s okay, maybe you’ll tell me later.”
Very often, people hide suicidal ideas and attempts because they know that the threat of suicide is a strict indication for hospitalization. Sometimes the patient admits that he had such thoughts only after a few weeks, when he feels better. In such cases, I thank people for their honesty - because it’s not easy to talk about suicidal thoughts and self-harm.
There is a lot of personal in the relationship between a doctor and a patient - patients transfer the model of relationship with their parents onto the doctor. For example, if they have the thought in their head: “Dad won’t accept this,” they won’t tell the doctor about the same thing. Hence the legend about “old psychiatrists who won’t understand this.” Young patients find it a little easier to communicate with young doctors.
— At what point does a patient who did not trust the doctor begin to trust?
— There are no special magic words. You simply create an atmosphere of trust. Sometimes a person is captivated by the very fact that he can sit with a doctor, tell him something very personal, and the doctor calmly, carefully listens to him and is not “terrified.”
Sometimes you can say: “In your situation, people usually experience these feelings and think about this.” Although some people perceive this as a threat: “A person sees me for the first time in his life, and already looks right through me?” Other patients, on the contrary, are glad that they are understood and open up.
There is a difficult issue with shame: during an exacerbation, a person can commit socially unacceptable acts - fight, undress, swear. And the doctor at the appointment cannot shame him for this, educate him, moralize him, otherwise he will simply lose contact with the person, the person will hide himself as “that way.”
But the main thing is to listen and let them talk. Yes, healthcare exists within the framework of eternal time pressure. But it is important to allow the person to speak out at the initial appointment. Believe me, he will tell you much more this way than answering leading questions every thirty seconds. Sometimes I really want to interrupt the patient, and I stop myself with an effort of will.
Sometimes it is very useful to ask a person how he sees his condition.
That is, to turn not to his patient’s experience, but to his everyday experience: what is happening to him, from his point of view, is it a disease or not a disease, normal or not normal?
The third way, oddly enough, is to discuss treatment options with the patient. Because otherwise it turns out “the doctor prescribed pills, well, since he is so smart, let him take them himself.”
Ideally, we should offer the person treatment options and tell them about all the side effects. So that the patient comes to the doctor not as a guru in a white coat, but can talk to him as an equal.
Yes, the doctor has experience of treatment, but the patient has experience of the disease. The paternalistic model of relationships that existed between the doctor and the patient before is now not liked by all patients.
Some people find directive guidance from a specialist very comfortable, and the doctor should come “from the patient.”
If the patient says, “Doctor, decide for yourself,” you decide. If a person wants to discuss his condition, you discuss it in detail. It is very important for someone to know their diagnosis, discuss the details of treatment, and offer their options.
Such a person brings books to the appointment and says: “I think I have bipolar affective disorder. And you sit and explain why it’s not so.”
For others, the diagnosis is not important, but what is important is to pull together and overcome the disease.
Organization of reception
Those who have never visited a psychotherapist are worried about how the appointment goes. First of all, you need to consider your work style. One plays relaxing music for the patient, another uses aroma lamps, the third is no different from an ordinary doctor. Therefore, despite the presence of a general outline for at least the first consultation, there will always be nuances that cannot be predicted.
The first reception goes something like this:
- Acquaintance.
- A schematic, superficial presentation of the main problem.
- Leading questions that allow you to delve into the essence of a psychological problem and understand the reasons for its occurrence.
- Diagnosis of physiological condition: pulse, blood pressure, excess weight, complaints of headache or insomnia.
- Finding out the patient’s goals, desires and plans (what he expects from the course of treatment).
- Initial diagnosis.
- Developing a strategy for the future: choosing a direction, basic techniques, techniques, frequency of techniques.
- Prescribing medications for treatment, referrals to other specialists.
After the first appointment, the doctor must analyze the collected information, draw appropriate conclusions, and possibly adjust the diagnosis, course of treatment, and selected techniques and methods. All this is agreed upon with the patient at the next visit and therapy begins directly.
If the patient leaves the appointment calmed, peaceful, or at least with the feeling that the ice has been broken, time was well spent. Sometimes there is disappointment - in such cases you should not draw hasty conclusions. Perhaps this is just the first consultation, and a second one is needed to ensure the professionalism of the psychotherapist.
Question answer. How long does the appointment last? Primary - from 50 minutes to 1.5 hours. Subsequent ones - about an hour, in accordance with the chosen direction, form of work and technique. Frequency: 1-3 times a week. The average course of treatment is 10 sessions. Numbers may vary depending on the diagnosis and severity of the condition.