This type of mental illness may also be called psychosis or paranoid symptom in medical practice. It is characterized by the presence of delusions in the patient, which are characterized by systematization. The patient is convinced that there is something false. At the same time, the perceived false is devoid of imagination and whimsicality. Among the manifestations there are the following variants of delirium:
- jealousy;
- persecution;
- dysmorphophobia;
- sensations of unrequited love and others.
Often the perceived manifestations are noticeably exaggerated or completely untrue. Diagnosis of the pathology is complicated by the variability of manifestations. Experts identify several of the most common manifestations.
Development of the disorder and the nature of the patient’s actions
The development of the syndrome may continue for several years.
The person is closed, all his attention is directed to himself. The patient sees others as a threat and an unfriendly attitude towards himself. As a rule, others evaluate such an individual as a self-centered person with high self-esteem, closed and distant from reality. The delusional state develops gradually with small ideas. Delirium can be systematized. In this case, the patient can prove what his fears are based on. When a delusional idea is not systematically manifested, the patient is lost and cannot explain the reason for suspicion, but also sees everyone as an enemy and a persecutor. Delirium of persecution occurs without clouding of consciousness.
The patient’s firm belief that enemies are watching him and using certain actions to control a person’s thoughts, desires and actions is called Kandinsky-Clerambault syndrome or mental automatism.
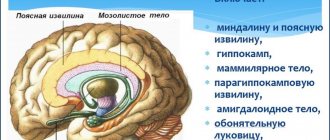
Mental automatism is divided into three groups according to the nature of the apparent impact:
- Associative (ideational) . The patient is convinced that his ability to think freely has been taken away. He believes that his pursuers know what he is thinking about.
- Senestopathic . This type is characterized by painful painful sensations. The patient is convinced that the pursuers cause pain by influencing internal organs. Through influence, enemies, for example, force you to restrain your heart rate or urination.
- Kinesthetic (motor) . Characterized by the manifestation of motor acts. Sometimes associative automatism is added to motor automatism. This form is the most complex of all manifestations of automatisms; speech motor hallucinations are noted in it.
Patients try in every possible way to “protect themselves” from their enemies. They write numerous statements asking to be protected from persecution and sew protective clothing. Their actions become dangerous to others. For example, they can destroy electrical wiring in an apartment so that enemies cannot use their devices.
Are common
This syndrome includes tactile hallucinations in combination with visceral ones. In this case, the patient sees moving objects in the surrounding reality that cause him discomfort. Sometimes imaginary objects can be on his body, and sometimes inside, in the internal organs. As a rule, the patient begins to see worms and insects. Some people are tormented by visions of frogs, imaginary fairy-tale creatures, such as dragons.
This kind of vision is quite persistent. Often, a patient is treated by many doctors, complaining of all sorts of symptoms, undergoes several courses of therapy, and then ends up seeing a psychiatrist. In medical practice, cases have been recorded when a patient complained of a frog sitting in the stomach. The symptoms disappeared only when the psychiatrist induced vomiting in the patient and put a frog in the vomit.
Something similar develops in those who suffer from senestopathy. In this case, there is no separate set of uncomfortable sensations. The patient complains of pain, heaviness in the body, but does not associate them with a specific object - insects, stones, any creatures, as happens in people suffering from hallucinosis.
Gustatory and olfactory hallucinations are very rare. As a rule, they are not symptoms of any mental disorders.
Where does the disorder begin?
Until now, medicine has found it difficult to name the exact cause or complex of provoking factors.
The phenomenon can have a very different etiology. The syndrome is formed on the basis of genetic predisposition, congenital or acquired diseases of the nervous system, which are characterized by changes in the biochemical processes of the brain. In cases of the use of narcotic or psychotropic drugs, or alcohol abuse, the cause of the paranoid syndrome is clearly defined. A short-term phenomenon of paranoia can be observed in people under the influence of prolonged severe stress.
Those at risk of developing this deviation are primarily patients with chronic mental illness (most often schizophrenics), sometimes patients with organic lesions of the brain and central nervous system (encephalitis, cerebrovascular disease, and others).
Medical statistics indicate that paranoid syndrome is most often observed in men.
And the first symptoms of deviations can appear at a young age (from 20 years).
In some cases, there is a rapid increase in characteristic symptoms.
Causes
The reasons for the formation of paranoid syndrome are not precisely determined. It is believed that its development can be triggered by the following factors:
- Psycho-emotional state disorder,
- Genetic predisposition,
- Stressful situations,
- Congenital or acquired neurological pathologies,
- Impaired metabolism of neurotransmitters,
- Taking psychotropic and narcotic substances,
- Alcoholism.
Acute paranoid is observed in schizophrenia, manic-depressive psychosis, organic damage to the brain and central nervous system caused by encephalitis or syphilis. This syndrome is a manifestation of reactive, symptomatic, alcoholic and other intoxicating psychoses.
According to statistics, pathology develops more often in men and first appears at the age of 20-30 years.
Clinical picture
Due to the isolation and suspicion of patients, difficulties arise in diagnosing mental disorders. There are a number of indirect symptoms by which paranoid syndrome is diagnosed:
- constant suspicion towards colleagues and friends;
- conviction that everyone around you is conspiring against you;
- inappropriate attitude towards harmless remarks, search for a hidden threat in them;
- severe grievances;
- suspicion of loved ones of betrayal and infidelity.
Subsequently, auditory hallucinations, persecution mania, secondary systematized delusions develop (the patient clearly explains how and on what day the surveillance began, and how it manifests itself) and sensory impairment.
Paranoid syndrome progresses along delusional or hallucinogenic paths of development. The delusional nature of the disorder is more complex and requires long-term treatment. The reason is the patient’s reluctance to contact anyone. Hallucinogenic can occur as an acute mental disorder. It is classified as a mild form of deviation due to the patient’s communication skills. The prognosis for treatment is quite optimal.
Manifestations of mental disorder are expressed in various forms.
Chronic delusional disorder
In chronic delusional personality disorder, persistent delusions become a persistent symptom. It accompanies a number of mental disorders. They can be characterized as:
- schizophrenic;
- affective;
- organic.
A single picture of delirium or a series of interconnected pictures develops. They can last about three months or be lifelong. The forms of the disease are varied. At the moment, experts identify several leading ones:
- Paranoid syndrome, in which delusions are not accompanied by hallucinations. Delusional states change personality, but in this situation they do not have signs of dementia, due to which patients often seem completely normal to others.
- Paranoid syndrome, in this case, delusion fits into a certain system, but is less logical and more contradictory. Hallucinations become persistent. Patients constantly hear voices in their heads. Without treatment, it leaves an imprint on your professional and personal life.
- With Paraphen syndrome, delirium becomes obsessive, fantastic, fictitious.
Determination of the type of condition is carried out only by a doctor. As well as developing a course of treatment.
Delusional disorder treatment
Therapy includes psychotherapy and medication. It is psychotherapy that turns out to be more effective, as it allows you to solve behavioral and psychotherapeutic problems. After the courses, the patient begins to control his condition and behavior. Family therapy becomes a mandatory step.
The pathology is chronic. Long-term remissions are possible. In some cases, complete recovery is noted.
Organic delusional schizophrenia-like disorder
The disorder is not of endogenous origin. Manifestations lead to the formation of a schizophrenic effect. With this lesion, the following is formed:
- pretentious nonsense;
- delusional disorders of a religious type;
- interpretive nonsense.
Hallucinations are a common secondary manifestation. An astatic and depressive-dysphoric affect occurs. During treatment, medications are used that are determined by the physician.
Hallucinatory delusional disorders
With this lesion, a characteristic feature is the presence, in the complete absence of signs of confusion, of pronounced delusional and hallucinatory disorders. Among the differences:
- confusion;
- severe anxiety;
- motor excitations.
All these manifestations are caused by the constant presence of hallucinations, which are short-lived and occur without provoking factors. They have acute and chronic forms. As the hallucinations become chronic, they become monotonous. The patient adapts to his condition and the pathology becomes less visible to others. The individual distances himself from violations.
Acute delusional disorder
Delusional disorder does not have an organic form. Delirium is devoid of bizarreness. The paranoid personality structure becomes a provocateur. The number of confirmed diagnoses increases in families where there are people with schizophrenia. Due to sthenicity, patients often convince others of the reality of delusional manifestations. Patients often suffer from persecution syndrome and change their place of residence. They are inclined to join heretical sects due to religious ideas and ideas of greatness. The object of love is often chosen by famous stage personalities who do not know about the object experiencing love. A factor confirming pathology is the presence of delusional ideas, the duration of which exceeds three months. Delusions and hallucinations do not meet the criteria for schizophrenia.
Affectively delusional disorder
Disorders associated with disturbance of affect, involving disturbances in the emotional state. They include several pathologies, the most well-known of which are bipolar or major depressive disorder. Often characterized by the manifestation of inappropriate emotions.
The classification is divided into several types of disorders:
- depressive spectrum;
- bipolar spectrum;
- manic spectrum.
Doctors often associate the presence of affective delusional disorder with creativity.
Induced delusional disorder
The pathology initially occurs in a person who is part of a close circle of relatives or friends. The patient in this situation becomes only a recipient, transmitting delusional ideas and disorders of the dominant. Moreover, a mental disorder in this “pair” is present only in the dominant personality. The recipient only copies the behavior and thoughts of the leader.
The couple is often isolated from the outside world. Only the recipient maintains minimal contact. The danger becomes the indignation experienced by the dominant when there is excessive adoration. Such relationships can occur in the same family. Recipients are often women. The patient is unable to distinguish between reality and his own view of the world, accepted from the dominant one.
Hallucinatory-paranoid syndrome
In addition to the patient's feeling of constant surveillance with the aim of causing harm to health or even murder, this condition is characterized by hallucinations and pseudohallucinations. Most often, this condition occurs after a severe affective disorder, manifested in aggression and neurosis (hence the second name affective paranoid syndrome). There is a strong constant feeling of fear and a variety of delusional ideas.
This condition is characterized by consistent development. The stages of formation of paranoid syndrome of the hallucinatory type have a certain order:
- rapid change of emerging thoughts, the patient has a strong belief that outsiders can read his thoughts and influence them;
- the next stage is characterized by increased heart rate, which the patient feels, withdrawal symptoms, convulsions and hyperthermia;
- at the final stage of this form of pathology, the patient gains confidence in controlling his subconscious from the outside.
In each of these stages, hallucinations appear in the form of unclear images or blurry spots. The patient cannot describe what he saw, but he is convinced of an outside influence on his thinking.
Clinic
Often patients with the syndrome do not make contact with a doctor, so it is simply impossible to talk with them and find out their complaints.
Patients are suspicious of friends, family and close people, they speak sparingly and for a long time, thinking about every word. They react sharply to simple remarks and statements addressed to them by others, are overly touchy, jealous and confident in betrayal, conspiracy, and infidelity. These are indirect signs of the syndrome, on the basis of which doctors usually make a diagnosis. As the pathology develops, auditory hallucinations, persecution mania, and disturbances in the functioning of sensory systems are added.
Hallucinatory-paranoid syndrome
This syndrome is a severe mental disorder manifested by the following symptoms:
- The feeling of the constant presence of strangers watching the patient and wanting to hurt him or even kill him,
- The occurrence of hallucinations and pseudohallucinations,
- Aggression and neurosis,
- Constant feeling of fear
- Various nonsense.
Patients are confident that those around them know their thoughts. This confidence often reaches the point of absurdity: patients feel that the thoughts in their heads belong to strangers. Patients' pulse quickens, convulsions occur, and body temperature rises. They realize that they are under the control of other people and are no longer their own. “Someone” controls their consciousness. Under the influence of an outside force, pictures, images and spots appear in their thoughts, which they clearly see.
As this form of pathology develops, patients develop mental automatisms. First, associative automatism is formed - rapidly arising thoughts in the head that “everyone knows about.” Then sensory automatisms appear - these are unpleasant sensations of pulsation, twisting, heat. Motor automatisms are the compulsion to submit to other people’s thoughts.
Video: film about hallucinatory-paranoid syndrome
Depressive-paranoid syndrome
Symptoms of this form of pathology are:
- Depression,
- Depression,
- Sleep disturbance, insomnia,
- lethargy,
- Unbearable sadness
- Lack of joy in life
- Decreased self-esteem, appetite and libido,
- Thoughts about suicide
- Lack of meaning in life
- Rave,
- Exhaustion of the patient
- Blood pressure disorder
- Cardiac dysfunction.
There are four stages in the development of this form of pathology:
- Cyclothymic - general depression with decreased self-esteem, loss of joy in life, pessimism, decreased libido.
- Hypotymic – melancholy, despondency, sadness, lack of desire to live.
- Melancholic - the transition of moral pain into physical pain, suicide attempts.
- Delusional – delirium of self-blame and sinfulness. Patients blame themselves for all tragedies and cataclysms. These thoughts lead them to suicide.
The disease lasts 2-3 months and is difficult to treat.
Manic-paranoid syndrome
The syndrome manifests itself:
- Unreasonable increase in mood,
- Hyperactivity and hypermobility of patients,
- Mental agitation,
- Fast thinking and reproduction of thoughts,
- Pursuit of the opposite sex
- Causing physical injury to others,
- Constant aggression and distrust of loved ones,
- Increased sexuality and appetite,
- Reassessment of your personal qualities.
Manic-paranoid syndrome occurs under the influence of alcohol or drugs . It is caused by emotional outbursts or extreme stress. Such patients are dangerous to others.
Alcoholic paranoid deserves special attention. Indeed, it is currently considered a serious disorder that develops in the majority of patients who are admitted to the clinic with psychosis due to alcoholism. It ranks third in patients with alcoholism after delirium tremens and hallucinosis. The disease requires immediate hospitalization and long-term rehabilitation therapy. Most often, alcoholic paranoid is diagnosed in alcoholics who have suffered a head injury, have severe heredity, or suffer from epileptoid psychopathy. The pathology manifests itself through sudden mood swings, sensual delirium and inappropriate behavior.
Depressive disorder
Symptoms of depressive-paranoid syndrome are expressed as follows:
- there is a decrease in self-esteem, the joy of life disappears, there is no sexual desire;
- the patient develops suicidal tendencies;
- then an obsessive idea of suicide appears;
- delirium is noted in all manifestations.
This condition often occurs against the background of complex mental trauma. Depressed state and depression lead to sleep disturbances, and then to its complete absence. There is inhibition in behavior. This condition develops within 3 months. The patient suddenly loses weight and develops problems with the cardiovascular system.
Diagnostic criteria
Due to a decrease in the patient’s communication skills, the diagnosis may not be made immediately, but after long-term observation and a series of psychological tests.
The syndrome is differentiated with a number of organic changes, such as dementia, as well as with stress and affective changes in epilepsy.
Particular attention is paid to little things, the specificity of experiences is assessed - overestimation of personality and excessive detail distinguish paranoid syndrome from similar signs of disorders of other etiologies.
Treatment approach
Treatment of paranoid syndrome requires hospital conditions.
Relatives of the patient should understand that early detection of pathology plays an important role in the prognosis of treatment. This condition does not go away on its own, but is characterized by an increase in symptoms. The therapy program is selected individually in each case. The doctor prescribes antipsychotic drugs (Aminazin, Sonapax, Triftazin, etc.), with the help of which the patient is brought into a stable state of mind. The timing depends on the degree of the disease and can range from one week to one month.
Therapy started at the first manifestation of dangerous symptoms has a good effect. The patient is quickly returned to a stable mental state. If treatment is delayed, the situation worsens and treatment takes longer.
Relatives of the patient need to know that it is impossible to achieve a complete recovery in such patients. But under certain conditions, loved ones can prevent further deterioration of the disease.
Hallucinatory-delusional psychoses
Darkness or cloudiness of consciousness in the current case often manifests itself in two forms: hallucinatory and paranoid. Men are more often susceptible to hallucinatory-delusional psychoses, and they arise as a result of moderate or severe traumatic brain injuries. Often, many years have passed since the injury occurred, which may explain the average age of patients - forty years or more.
The development of such psychosis occurs in an acute form, usually turning into chronic. The onset is characterized by various types of confusion with bouts of delirium and verbal hallucinations. Subsequently, the leading role in the attacks is occupied by hallucinatory delusions with the syndrome of verbal hallucinosis.
The course of the disease also passes in a paroxysmal form, replaced by periodic reductions and a reduction in hallucinosis, due to which the attacks are shortened. Sometimes paranoid disorders are present in reducing attacks, but in most cases the psychosis stops at the hallucinatory stage.