What is the peripheral nervous system?
The human nervous system is divided into 2 large sections: central and peripheral. The first includes those structures that are located in the brain and spinal column. The second includes nerves located outside the brain and spinal cord.
The peripheral nervous system (PNS) connects them with receptors (sensitive formations) and effectors (end processes of nerve cells that transmit nerve impulses to organs). As a result, adaptive reactions of the body occur, for example, contraction of muscle tissue or secretion of secretions.
Part of the peripheral nervous system is the somatic one, which supplies the skin, muscles, bone apparatus, and some internal organs with nerves. Thanks to it, interaction with the external environment is carried out. Another component of the PNS is the autonomic system, which innervates the organs. It regulates internal processes occurring in the body.
The structure of the peripheral nerve
The peripheral nervous system is an extensive network consisting of many nerve endings and nodes that cover all organs and areas of the human body. The nerves connect to the central nervous system, located in the spinal cord and brain. Information received from the peripheral nerve is processed by the brain and sends a command for a specific action.
Depending on the type, location, and functions performed, peripheral nerves are divided into:
- Sensory. They innervate organs and areas of the body that are responsible for sensory perception (skin, ability to see, hear, etc.).
- Motor (motor). Provide innervation to the muscles that provide movement of the limbs, head, and speech muscles.
- Autonomic nerves. With their participation, vital processes occur in the body, for example, maintaining normal blood pressure, breathing, and the functioning of the internal secretion organs.
Damage to the peripheral nerves in a certain part of the body disrupts the well-functioning mechanism and leads to peripheral neuropathy or polyneuropathy, which is expressed in partial or complete loss of sensitivity.
What is peripheral neuropathy?
Peripheral neuropathy is damage to the nerves. Since the PNS covers almost the entire human body, the manifestations of peripheral neuropathy can be very different. This is not a separate disease, but a whole symptom complex that is associated with different conditions.
The lesion is based on degenerative processes that lead to damage and destruction of nerve fibers (their sheaths or rods - axons). They can occur due to several factors described below. The most common symptoms are pain, sensory disturbances, and muscle weakness.
How does neuropathy develop?
Peripheral nerves originate from the spinal roots (vertebral nerves) and the brain (cranial nerves). The spinal cord roots also belong to the elements of the peripheral (located outside the brain and spinal cord) nervous system, but the symptoms of their damage are called “radiculopathy” and are considered separately from neuropathy.
Contents of the article: Classification Causes of development How it manifests Treatment methods
Numerous branches of the peripheral nerves provide innervation to all tissues and organs, transmitting nerve impulses to the brain that regulate the activity of the body from the most distant points (feet and hands) and back.
Groups of fibers within the branches of the nerve perform their highly specialized functions:
- somatic: sensory (sensitive);
- motor;
Sensory (afferent) fibers are responsible for all types of sensitivity of body tissues. Motor (motor, or efferent) fibers provide motor function - walking, working with the hands, movements of the head and torso. Vegetative fibers are responsible for the coordinated functioning of internal organs, glands, and blood vessels.
Damage and destruction of peripheral nerves under the influence of various unfavorable factors leads to disruption of these functions - neuropathy. Neuropathy can manifest itself as pain, sensory disturbances, limited mobility, and functional disorders of various organs and systems.
What is affected?
PNS neuropathy can damage the following parts of the nervous system:
- 12 pairs of cranial nerves leaving the brain at its base. These include the olfactory, vagus, visual, oculomotor, trigeminal, glossopharyngeal nerve and others. Accordingly, when they are violated, the organs of the head suffer. The vagus nerve also provides communication between the central nervous system and organs located in the neck, chest and abdominal cavity (excluding the pelvis).
- 31 pairs of spinal nerves , which are grouped into 5 segments - cervical, thoracic, lumbar, sacral, coccygeal.
- Nerve plexuses – cervical, shoulder, lumbar, sacral.
Peripheral neuropathy
With peripheral neuropathy, the transmission of impulses from parts of the body to the brain is disrupted. Based on symptoms, there are 4 main forms of such disorders. In the most severe cases, vital processes such as breathing and heart function may deteriorate.
Epidemiology
The average prevalence of peripheral neuropathy in different populations is 6-7%. It occurs much more often than the central one (80-95% of cases). Different conditions have different chances of developing neuropathy.
Thus, damage to the peripheral nervous system is observed in 20-40% of patients with diabetes mellitus. In acute herpesvirus infection, it develops in 20-45% of cases. In cancer patients in the last, terminal stage, this figure reaches 90%.
In some cases, clinical signs of damage to the nervous system become noticeable 5-10 years after the onset of the underlying disease. In 10% of patients with diabetes, diabetes itself is detected only after the first neurological symptoms.
Causes of peripheral neuropathy
In most cases, the pathology develops against the background of alcohol dependence or intoxication, diabetes mellitus and Guillain-Barré syndrome (an acute inflammatory process of autoimmune etiology). Minor factors that cause peripheral neuropathy include:
- inflammatory processes, injuries or compression (compression) of nerve endings;
- hereditary predisposition to diseases of the nervous system;
- HIV and other immunodeficiency conditions;
- autoimmune processes (rheumatoid arthritis, etc.);
- severe renal failure;
- diseases of hematopoiesis and blood vessels;
- malignant neoplasms;
- acute infectious diseases;
- hormonal and endocrine disorders;
- long-term exposure to heavy metals, radiation and other negative factors on the body;
- the use of certain medications (for example, chemotherapy drugs, anticonvulsants, antihypertensives, antibacterial agents);
- lack of vitamins due to an unbalanced diet;
- mental disorders.
In addition, there is an idiopathic type of the disease, when the exact cause of its development cannot be established.
Reference : 90% of patients are diagnosed with congenital peripheral neuropathy, and the acquired form is much less common, and, as a rule, it develops against the background of taking medications and complications of cancer.
Causes
Peripheral neuropathy is a pathological condition, the causes of which can be generalized into several large groups:
- injuries;
- endocrine disorders - insufficient or excessive thyroid function, diabetes mellitus;
- metabolic diseases - chronic renal or liver failure, a disorder of protein metabolism, in which the protein-polysaccharide complex of amyloid is deposited in the tissues (amyloid polyneuropathy);
- diseases of internal organs (obstructive pulmonary disease, gastrointestinal pathologies accompanied by malabsorption and deficiency of B vitamins);
- systemic pathologies of connective tissue - periarteritis nodosa (inflammation of the walls of arterial vessels with the formation of microaneurysms, or “nodules”), systemic lupus erythematosus (immune complex damage to connective tissue), scleroderma (an autoimmune disease in which blood microcirculation is disrupted, inflammation occurs and functional tissues are replaced fibrous);
- pathologies of the circulatory system - the appearance of abnormal proteins in the blood (with myeloma, tumors and other diseases);
- malignant neoplasms;
- toxic poisoning and taking certain medications (including alcohol abuse, drug addiction, lead intoxication);
- infectious diseases, vaccination and immunodeficiency conditions.
Injuries
When injured, the integrity of the nerve fibers is disrupted. The potential for recovery, which is inherent in peripheral nerves from the moment a person is born, is greatly limited. Therefore, severe injuries often lead to permanent loss of performance. In case of fractures, displaced bones also cause compression or compression of the spinal nerve roots.
Disruption of the PNS can also occur due to overexertion of the arms, which is associated with work activity. In this case, local trauma to the nerve endings of the palms and fingers occurs. This is facilitated by industrial vibration and exposure to chemicals (solvents, lubricants, etc.).
Alcohol and toxins
Alcoholic polyneuropathy leads the structure of toxic neuropathies. It is observed in 12-30% of patients suffering from chronic alcoholism, and in a latent (hidden) form is found in 97% of people who abuse alcohol.
The most common types of poisoning are:
- lead, which causes movement disorders;
- arsenic - the use of drugs to kill insects, medications, as well as when melting metal (manifests itself in the form of muscle weakness, sensitivity disorders);
- organophosphorus substances, which are part of insecticides, lubricants, and polymeric materials.
Infections and autoimmune diseases
Among all infectious diseases, neuropathy most often occurs in severe form with HIV infection. Various variants of symptoms are observed in 20-35% of cases, but at autopsy, signs of damage to the PNS are detected in 95% of patients.
The prevalence of neuropathy is also high in the following infections (the average number of patients in %) is indicated in parentheses:
- diphtheria (20%);
- tick-borne borreliosis (up to 40%);
- herpes (up to 45%);
- viral hepatitis (up to 42%);
- leprosy (up to 95%).
Medications
The development of neuropathy can be caused by taking medications such as:
- drugs used in chemotherapy - cytostatics for the treatment of tumors (Vincristine, Bortezomib and others);
- platinum-containing drugs, also used for malignant tumors;
- antiarrhythmic drugs (Amiodarone);
- antihypoxic drugs (Pergexiline);
- anti-inflammatory drugs (Chloroquine, used for malaria, amebiasis, systemic lupus erythematosus, rheumatoid arthritis, photodermatoses);
- antiprotozoal, anthelmintic drugs.
Causes
There are many nerve fibers of the peripheral nervous system in any part of the body, so peripheral neuropathy can occur with certain pathologies or injuries:
What leads to the development of the disease:
- Injury. Fractures, bruises, and cuts lead to damage to tissues and nerve endings, causing pain.
- Diabetes. The disease is systemic; high blood sugar has a negative effect on the entire body. The endocrine system is inhibited, metabolic processes in tissues deteriorate. These phenomena, occurring over a long period of time, become a common cause of the development of diabetic neuropathy or polyneuropathy.
- Addiction to alcohol. Even one-time consumption of alcohol depresses the nervous system. Alcoholism leads to malfunction of vital organs: kidneys, liver, digestive system, and negatively affects metabolism. Alcoholic neuropathy and polyneuropathy develop. In addition, when drinking alcohol, the body suffers from a lack of vitamins, which is also one of the factors of neuritis. With chronic toxic effects on the nerves, the upper and lower extremities are primarily affected; signs of the disease appear in the form of paresthesia, increased or, conversely, decreased sensitivity of the legs and hands, changes in their color, intense, burning pain.
- Malignant tumors. Tissue proliferation affects the nerves of the peripheral system, causing pain.
- Intoxication of the body over a certain period of time with pesticides, heavy metals (arsenic, cadmium, lead), radiation damage, exposure to other chemicals.
- Systematic use of medications that have significant side effects on the nervous system (anticonvulsants, antibiotics).
- Infectious diseases and autoimmune disorders. A number of infectious diseases cause inflammatory processes in tissues and affect nerve endings. Herpes zoster and the Epstein-Barr virus cause complications by affecting the nerve fibers that are responsible for the sensitivity of organs, leading to postherpetic neuralgia. The pathology is accompanied by intense pain. Factors affecting the peripheral and central nervous system are HIV infection, Lyme disease, the causative agent of which is bacteria from the genus Borrelia. These diseases can cause polyneuropathy of varying intensity and depression of the nervous system. Autoimmune disorders affect the myelin sheaths of peripheral nerves, which are the immune system's response to the action of a pathogen, thereby causing painful neuropathy.
- Hereditary factors.
Types, forms, symptoms
Peripheral neuropathy can manifest itself in several forms. This is due to the individual characteristics of the course of the disease and the variety of etiological factors.
The following forms of neuropathy are distinguished:
- sensory;
- motor;
- vegetative;
- mono- and polyneuropathy.
Sensory neuropathy
The following symptoms are characteristic of sensory (or sensory) neuropathy:
- change in skin sensitivity (increase or decrease);
- sensation of itching, tingling, burning, numbness, crawling “goosebumps” in the feet or hands;
- false feeling of a foreign body in shoes;
- insensitivity to high or low temperatures, which can result in burns and other types of injury;
- pain that occurs even with a light touch;
- formation of ulcers due to minor trauma to the skin;
- deterioration of reflexes.
Motor neuropathy
Motor (or motor) neuropathy manifests itself as follows:
- deterioration of fine motor skills - awkwardness when writing, tying shoelaces, fastening buttons, difficulty grasping and holding small objects;
- uncertainty when walking, stumbling, uneven gait, difficulty getting up from a sitting position;
- muscle twitching, involuntary movements, convulsions;
- muscle weakness;
- in severe cases - paralysis.
Autonomic neuropathy
Symptoms of the autonomic form of neuropathy include:
- decreased (dry skin) or increased sweating;
- changes in intestinal motility (diarrhea or constipation);
- urinary incontinence;
- hearing impairment (decreased hearing, sensation of noise or ringing in the ears);
- dizziness;
- tachycardia, arrhythmia;
- impotence in men.
Mononeuropathy
In mononeuropathy, only one motor, sensory or mixed nerve is affected. For example, neuropathy of the facial nerve manifests itself in paralysis of the facial muscles. This condition can occur with severe hypothermia.
Mononeuropathy is most often associated with peripheral nerve compression or toxic effects, which leads to impairment of its functions to varying degrees.
Polyneuropathy
Damage to two or more nerves is called polyneuropathy. In European countries, its most common cause is diabetes mellitus. Damage to nerves occurs as a result of disruption of their blood supply, biochemical reactions (addition of sugar to the protein membrane of neurons) and other pathological processes.
Diabetic polyneuropathy is characterized by the following manifestations:
- absence or decreased reflexes in the lower extremities;
- diabetic foot syndrome (formation of long-term non-healing ulcers on the legs);
- loss of tactile and vibration sensitivity;
- muscle atrophy and other disorders.
Symptoms of the disease
The symptoms of the disease are caused by damage to the nerves that perform certain functions in the body.
Depending on the cause of the nerve damage, signs of peripheral neuropathy appear almost immediately or after several years.
The nature of the damage can affect different types of peripheral nerves simultaneously (sensory, motor, autonomic) or separately:
- Sensory peripheral neuropathy is characterized by numbness of the extremities, decreased sensitivity to pain, and impaired coordination, which leads to loss of balance.
- Motor neuropathy is manifested by muscle weakness, muscle cramps, paralysis, paresthesias that affect one or a group of muscles. Due to weakness in the hands, sometimes it is not possible to hold objects in the hands.
- Idiopathic peripheral autonomic neuropathy is dangerous because it affects vital organs; failure of their functioning can have serious consequences. From the cardiovascular system - changes in blood pressure, accompanied by dizziness, tachycardia. Problems with the intestines arise, which are expressed in attacks of diarrhea, or, conversely, constipation, bloating, and nausea occur. The patient experiences problems with urination, sweating or decreased sweating. Men experience sexual dysfunction. There are problems with breathing and swallowing.
Peripheral neuropathy in children
In addition to the disorders listed above, there are a number of hereditary diseases accompanied by the occurrence of peripheral neuropathy:
- peroneal muscular atrophy , in which the myelin sheath of nerve fibers is damaged; the main symptom is atrophy of the muscles of the lower extremities;
- polyradiculoneuropathy is an autoimmune inflammatory pathology manifested in decreased muscle strength, deterioration of sensitivity, autonomic disorders (tachycardia, drop in blood pressure, arrhythmia, urinary retention, and others);
- Dejerine-Sotta disease , which is characterized by dystrophy of peripheral nerves; the onset of the disease occurs in the first years of life, leading to early disability of the child and other genetic disorders.
Most often, these pathologies are characterized by the formation of symmetrical, gradually progressive atrophy of muscle tissue.
Diagnostics
If symptoms of peripheral neuropathy appear, you should consult a neurologist. The diagnosis is made on the basis of a number of studies, which include instrumental and clinical methods.
- Primary medical examination . The doctor collects the patient’s complaints and medical history, and uses special tests to evaluate reflexes, balance, coordination, sensitivity and other indicators of muscle function.
- Analyzes . Blood tests are carried out to identify inflammatory and infectious processes in the body, measure the level of glucose and thyroid hormones, as well as the content of vitamins and microelements. Sometimes patients require genetic testing, lumbar function, and biopsy of skin, nerve, and muscle tissue.
- Electrodiagnostic testing . Electromyography is performed to evaluate the electrical activity of muscles and the speed of impulse transmission.
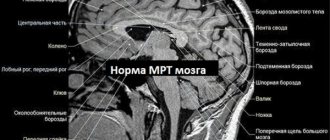
- Pictures . To identify lesions of internal organs, bone and muscle tissue, magnetic resonance and computed tomography are used - they allow you to obtain layer-by-layer images of the body's structures and identify almost any disorder, from mechanical injuries to benign and malignant neoplasms.
Some patients additionally require consultation with an endocrinologist, immunologist, infectious disease specialist and other specialized specialists.
Important : the symptoms of peripheral neuropathy are similar to those of other diseases (for example, fibromyalgia), so a diagnosis cannot be made without a comprehensive diagnosis.
Complications and consequences
Complications of peripheral neuropathy include:
- loss of heat or pain sensation;
- muscle weakness;
- spontaneously occurring pain;
- decreased reflexes, deterioration of motor activity;
- painful spasms;
- in severe cases – disability;
- sphincter insufficiency, involuntary urination as a result of loss of bladder muscle tone;
- impotence;
- in the cardiac form - orthostatic hypotension (a sharp drop in pressure when standing up, accompanied by dizziness, fainting), myocardial infarction, sudden death syndrome.
The most severe forms are characteristic of polyneuropathies that affect vital organs. Thus, when the latter type (cardiac) is diagnosed, up to 50% of patients die in the next 5-10 years.
When to see a doctor? Diagnostics
You should consult a doctor when the first signs described above appear, especially if you have a history of diagnosed chronic diseases in which this symptom complex may occur. At the first stage, you need to contact a therapist, who, if necessary, will refer you to a neurologist and other specialized specialists.
The diagnostic algorithm includes:
- studying the general condition of the patient, assessing reflexes and motor ability, collecting anamnesis;
- electrophysiological studies;
- biochemical tests.
Neurological examination
During a neurological examination, the following parameters are determined:
- superficial sensitivity (on both feet, legs, thighs, forearms, shoulders; with a cotton swab and a sharp object);
- deep sensitivity (vibration sensitivity, using a graduated tuning fork or biotensiometer applied to the thumb and ankle);
- cold sensitivity (metal and plastic);
- muscle reflexes on the limbs (using a neurological hammer);
- muscle strength.
Hardware, instrumental research
Instrumental diagnostic methods include:
- electromyography, which allows you to determine the electrical activity of muscle tissue (electrodes are attached to the surface of the skin or inserted as needles into it);
- electroneurography, which helps to assess the decrease in the speed of propagation of an electrical impulse and the action potential of nerve fibers (diagnosis of the functional state of peripheral nerves);
- MRI and CT scan of nerve fibers in the area of their supposed compression;
- ultrasound examination of nerves, which allows us to evaluate their structure and changes in characteristics.
Laboratory methods
The following laboratory methods are used:
- biochemical blood test (determination of thyroid hormones, erythrocyte sedimentation rate, glucose, protein, B vitamins);
- general urine analysis;
- biopsy of the sural nerve followed by histological examination;
- skin puncture biopsy to assess nerve fiber density, which is significantly reduced in neuropathy.
Classification of neuropathy
Depending on which area of the human body the nerves are damaged, neuropathy is distinguished:
- peripheral – with damage to the nerves of the arms or legs: distal – with localization of pain and other manifestations in the lower extremities: feet, legs, hands, forearms;
- proximal - with localization of painful symptoms in the upper part of the limb: thigh, buttock, shoulder;
The most common is distal peripheral neuropathy of the legs - these nerve fibers of this zone are most susceptible to adverse effects due to their distance from the center and large extent.
Depending on the severity of nerve damage, the following are distinguished:
- focal neuropathy – with damage to individual nerves: mononeuropathy – damage to a single nerve;
- multiple mononeuropathy - damage to several individual nerves;
Read also….
Silicone insoles: types, under what conditions to wear, where to buy and how to choose, cost Depending on what fiber specialization has undergone damage, neuropathy can be:
- sensory;
- motor (motor);
- vegetative;
- mixed (for example, sensory-motor).
Some nerves are made up of all three types of fibers, others are made up of just one type of fiber. Therefore, if one nerve is damaged, for example, only motor disturbances or sensory disturbances may be observed, or these symptoms may be combined.
Internal and local remedies
The prescription of certain medications depends on the type of disease against which the neuropathy developed. For example, in diabetes mellitus it is necessary to normalize blood glucose levels and constantly monitor them.
Metabolics, blood flow-regulating drugs
Antioxidant and metabolic agents help reduce the damaging effects of toxic and dysmetabolic effects. The main characteristics of these drugs are shown in the table below.
| Name | Main component | Pharmacological effect | Dosage |
| Actovegin | Deproteinized hemoderivative | Improving microcirculation, metabolic processes in cells, synthesis of carbohydrates and proteins. | At the first stage - 1.2-2 g per day (intravenously), subsequently - 600 mg 3 times a day (orally); long-term use. |
| Berlition | Alpha lipoic acid (thioctic acid) | Reducing the severity of oxidative stress. | 600-900 mg per day for 3 months (first intravenously, then orally). |
| Thioctacid | |||
| Thiogamma |
Vitamins
To restore nerve fibers and their myelin sheath, vitamin therapy with preparations containing vitamin B1 (thiamine), B6 (pyridoxine), B12 (cyanocobalamin), which are administered intravenously in the form of a solution or orally in tablets, is indicated. The average daily dosage for the first two drugs is 100 mg, and for cyanocobalamin - 100 mcg.
Painkillers
Peripheral neuropathy is a deviation that is almost always associated with pain.
For severe pain, it is recommended to take the following medications (daily dosage is indicated in parentheses):
- tricyclic antidepressants – Amitriptyline (25-150 mg in 2 doses);
- serotonin and norepinephrine reuptake inhibitors, or SNRIs - Duloxetine (60-120 mg per dose), Venlafaxine (37.5 mg 2 times);
- anticonvulsants – Gabapentin (1.2-3.6 g in 3 doses), Pregabalin (300-600 mg in 2 doses), Clonazepam (4-6 mg);
- opioid analgesic – Tramadol (50 mg once).
For pain of low and moderate intensity, non-steroidal anti-inflammatory drugs are prescribed - Diclofenac (100-150 mg in 2-3 doses), Ibuprofen (1.2 g), Xefocam (8-16 mg in 2-3 doses), Meloxicam (7.5 -15 mg), Ketorolac (10 mg up to 4 times a day) and others.
Nerve impulse stimulants
The drugs listed in the table below are prescribed as drugs that improve the conduction of nerve impulses.
| Name | Main component | Dosage |
| Prozerin | Neostigmine methyl sulfate | 15 mg 2 times a day |
| Galantamine | Galantamine | 10 mg 3 times a day |
| Ipigrix | Ipidacrine | 20 mg 2-4 times a day |
Homeopathy
The following homeopathic remedies are used:
- Traumagran;
- Coenzyme compositum;
- Discus compositum;
- Neuralgo-Reum-Inel;
- Traumeel S;
- Echinacea compositum.
Treatment
In case of neuropathies, first of all, it is necessary to find out their cause and treat the underlying disease that has a detrimental effect on the condition of the nerves - maintain a stable low level of glucose in the blood in case of diabetes, compensate for the level of thyroid hormones in case of its diseases, and so on.
Treatment of neuropathy itself is conservative and is aimed at eliminating pain, speedy restoration of the affected nerve tissue, and restoration of the functions of nerve fibers. However, without eliminating the root cause, such treatment does not provide a good long-term effect.
Read also…. Uncovertebral arthrosis of the cervical spine: symptoms and treatment
Drug treatment
In case of severe pain, non-steroidal anti-inflammatory drugs are used to relieve pain. If these drugs are ineffective, anticonvulsants, antidepressants, tranquilizers, and narcotic painkillers are prescribed.
To improve nutrition and speed up the restoration of nervous tissue, B vitamins are used in combination with ascorbic acid and vitamin E, vasodilators, and antioxidants.
To restore the functions of the affected nerves, anticholinesterase drugs are prescribed.
In some cases, for example with facial nerve neuropathy, the use of glucocorticoids is necessary.
Physiotherapy
Physiotherapy is prescribed to speed up the recovery of nerves and their functions, and relieve pain. In the treatment of neuropathy the following is used:
- electrophoresis;
- phonophoresis;
- magnetic therapy;
- diadynamic therapy;
- healing shower;
- therapeutic baths (radon, hydrogen sulfide);
- therapeutic mud, ozokerite;
- electromyostimulation.
Massage
Therapeutic massage also helps to improve nutrition of the affected nerves, relieve pain, and improve motor function.
Physiotherapy
Of the physiotherapeutic methods of treatment, the most effective is electrophoresis with drugs - the most often used are the anesthetic Novocain (5% solution) or the ganglion blocker Benzohexonium (2% solution, also for pain relief).
For vascular disorders, calcium and bromine ions are administered (in the form of solutions). Electrophoresis is carried out every day in 1 procedure lasting 15-20 minutes, the total duration of the course is 10 days.
In addition, the following treatment methods are used:
- application of an ultra-high frequency electric field (10 minutes every other day, course of treatment – 15 procedures);
- general exposure to ultraviolet light;
- baths with naftalan oil applied to the limbs (15 procedures every other day);
- plasmapheresis to cleanse the blood of toxins;
- acupuncture;
- hyperbaric oxygen therapy (reducing the effects of oxidative stress).
Physiotherapy
For dysfunction of the autonomic nervous system, the following complex of physical therapy is recommended:
- Starting position (i.p.) – standing position, legs spread shoulder-width apart, hands on the belt. Rise and fall on your toes.
- Alternately raising and lowering your legs with your knees bent.
- Circular rotational movements with legs half bent at the knees, in one direction and the other.
- As you inhale, raise your arms up, as you exhale, bend forward, and lower your arms.
- Circular movements of the pelvis.
- Squats (stretch your arms forward) as you exhale, return to i. p. while inhaling.
- I. p. - lying on your back. Rotate your feet first in one direction, then in the other.
- Alternately bend the legs at the knees, while the feet slide along the floor.
- Rotate your knees bent to the right and left.
- I. p. - lying on your stomach. Raise yourself on your hands, bending at the waist.
- I. p. - standing, feet shoulder-width apart. As you inhale, raise your arms up, hold your breath for 2-3 seconds, stretching upward, and as you exhale, lower your arms down.
- As you inhale, turn to the left, spreading your arms to the sides, then to the right.
- Bend back, putting one leg back, then the other.
All exercises are performed 4-6 times with a gradual increase in physical activity.
Folk remedies
In folk medicine, there are the following methods for eliminating nervous disorders:
- Treatment with blue clay. It can be used internally, for which you need to roll balls from wet clay and dry them in the sun. Clay has detoxifying properties, that is, it helps remove harmful substances from the body, and the complex of minerals in its composition helps restore the conductivity of nerve signals. Clay is also used externally as a wet application to a sore spot. To do this, it is diluted with water to a pasty state, applied to the skin and damp gauze is placed on top. The procedure is carried out every day until the composition dries completely, after which it must be washed off. The course of treatment is 2-3 weeks.
- For neuropathy of the facial nerve, it is recommended to eat 2-3 ripe dates. 3 times a day.
- If the sciatic nerve is damaged, massage with turpentine or camphor oil is performed. They have a warming effect, which improves blood microcirculation and tissue nutrition in the area of the damaged nerve. Massage is done every day or every other day, 10 procedures in total.
- You can also rub rosemary tincture on sore spots. For this, 2 tbsp. l. herbs pour 100 ml of vodka and leave for 2 weeks in a dark place. Then strain and rub the skin in the damaged area every day.
Precautions for people with peripheral neuropathy. Recovery prognosis
Precautionary measures for patients with neuropathy include the following recommendations:
- compliance with the work and rest regime (do not bring yourself to overwork);
- avoid infections, hypothermia;
- treat exacerbations of chronic diseases (sinusitis, pharyngitis, pyelonephritis, gastritis) in a timely manner to prevent a decrease in immunity;
- avoid contact with toxic substances (lead, varnishes, paints, solvents), do not abuse alcohol.
With timely treatment, the prognosis of the disease is favorable. In advanced cases, neuropathy can lead to disability and death of the patient. The most common form of PNS damage among patients of all age groups is peripheral polyneuropathy, that is, damage to several nerves.
This disorder requires different approaches to therapy, since its forms differ in etiology - genetic abnormalities, diabetes mellitus, alcoholism, toxin poisoning, infectious pathologies and other factors. Treatment tactics are aimed primarily at eliminating the cause of neuropathy.