Post-traumatic stress disorder is a delayed reaction to a traumatic event or emergency situation. Mental disorders can arise from PTSD; it is classified as a mental illness and is dealt with by a clinical psychologist or psychiatrist.
No one is immune from PTSD, because in essence it is the consequences of stress. But a special risk group consists of people in difficult professions, for example, military personnel, doctors. Although it is worth recalling the recent high-profile cases of the use of weapons in schools and shopping centers, and it becomes obvious that an emergency situation can arise anywhere. And even a certain style of family education can become a situation for a child that will cause PTSD in the future.
What is PTSD
In 1980, all the information accumulated on the topic of traumatic stress was combined, and a number of characteristic diagnostic criteria were identified for PTSD itself. PTSD can occur both in the object of external influence and in a witness of such influence (for example, a witness to a murder).
PTSD is an abnormal way of experiencing psychotrauma, dwelling on it instead of normal experience and recovery. PTSD creates irreversible changes in the physiological, mental, personal, professional, interpersonal and social aspects of a person's life. In this regard, the option of including post-traumatic personality disorders in the diagnostic criteria for PTSD is currently being considered.
What’s interesting is that the first changes can appear not only immediately after the injury, but even a long time after it, and progressing sharply and quickly. Cases have been recorded when war participants showed signs of PTSD 40 years after its end.
The essence of PTSD
What is PTSD? This is an abnormal experience of a traumatic event in which a person was a participant or witness, accompanied by physiological, mental, and social changes of an irreversible nature. According to ICD-10, PTSD is classified as a neurotic disorder associated with somotoform disorder and stress.
When a person finds himself in a stressful situation, he experiences fear and struggles to resist the influence of a negative factor. With normal adaptive abilities of the nervous system, the consequences of experiencing negative emotions disappear within a few days. But in about half of people who become hostage to traumatic events, the nervous system is so depleted that instead of reducing the negative consequences after the situation normalizes, post-traumatic stress disorder may become stronger. They associate events of normal life with a traumatic situation, they are in a state of stress, and experience panic attacks.
Today in psychology it has been established that a phenomenon such as PTSD can occur immediately after a traumatic event or after some time. For some combat veterans, symptoms of post-traumatic stress disorder appear many years after returning from the front.
Formation of PTSD
Psychotrauma occurs during, immediately after, or within two days after an unacceptable situation. From two days to a month, acute stress disorder develops, after a month - PTSD. Throughout life, pathological personality changes occur, that is, the development of post-traumatic stress disorder.
“Hole in the soul”, “emptiness in the soul”, “blackness in the soul” are popularly called PTSD. This is truly a heavy burden that a person brings in everyday conditions. But with this burden, normal life is no longer possible. It is extremely difficult to regain a sense of security and self-control, control over the situation. As a result, a person is in constant tension, which, of course, has a destructive effect on the psyche.
How does dwelling on trauma occur?
- A person wants to get rid of mental pain by forgetting the situation, ignoring what happened, and not trying to change something in himself. “I want to forget what happened,” he says.
- Over time, the experiences really seem to be forgotten, but in fact they pass into the subconscious, and do not go away completely.
- And all the same destructive emotions continue to influence, but on an unconscious level. From time to time, no matter how hard a person tries to avoid these emotions, they break out. As a result, the person loses control over himself and the situation.
- Outwardly, a person may look very prosperous, but the emotions accumulated inside will sooner or later make themselves felt.
- One smell, sound, or color reminiscent of a traumatic situation is enough for a person to plunge back into his worst nightmare, which was once a reality. This can happen again and again, naturally, it “breaks” a person and little by little he gets thrown out of the rut of life completely.
- The more often a similar situation occurs, the more a person tries to avoid similar circumstances, not to stumble upon irritating landmarks, guides to the world of the past. And it turns out that the trauma is constantly experienced. All thoughts are occupied with her: no matter how it happens again.
You can find guiding stimuli anywhere, which is why a person withdraws more and more into himself and four walls. Due to eternal control and avoidance, anxiety, insomnia develops, the functions of cognitive processes deteriorate, psychosomatic diseases arise, and a person becomes irritable. He ends up mentally and physically exhausted. Obviously, life in such conditions is more reminiscent of a dull existence.
Clinical picture
PTSD has main symptoms (3 of them) that are used to make a diagnosis, and accompanying signs.
Psychogenic amnesia
Since memories of a traumatic situation are too painful and have a destructive effect on the personality, the body turns on defensive reactions. As a result, a person begins to avoid those circumstances, people, actions and conversations that may remind of what happened. For example, after a terrible accident they do not get into cars, after the death of a loved one, they remove all his photographs from view and do not go to the cemetery.
For some, the trauma is so severe that the psyche, in order to cope with it, completely blocks memories. Thus, a participant in combat operations in a hot spot can talk in detail about his colleagues, about the smallest details of the campaign, but not about the battle where he lost all his friends (or was physically injured). This does not mean that he has forgotten - he simply subconsciously avoids such memories. This phenomenon is called psychogenic amnesia.
Involuntary experiences
Normally, psychological trauma for some time causes painful memories, which gradually fade, lose their brightness and relevance. A person with PTSD, despite all the memory blockages, is characterized by abnormal experiences of traumatic events over and over again. Moreover, he not only thinks about them, but practically feels everything the same: pain, fear, horror, disgust, fright, despair, helplessness, shock, shock and other negative emotions. They are so strong that they also affect the physical condition (increased sweating, tremors of the limbs begin, speech and motor functions are impaired, breathing becomes more frequent, and heart failure can be diagnosed).
One of the most obvious markers of post-traumatic stress disorder is the so-called “two thousand yard stare.” In psychotherapy, this term refers to a detached gaze directed into space.
These kinds of vivid intrusive memories significantly worsen the quality of life.
It is possible to cope with abnormal experiences of a traumatic situation caused by involuntary memories within a few minutes, especially with the help of loved ones. Some, who have a fairly strong type of nervous system, may not even show their emotions, although with such a diagnosis this is extremely difficult. All the same, at such moments you can see how he begins to worry, withdraws into himself, tries to isolate himself from others, does not answer questions, and is unable to carry on a conversation.
Reaction to triggers
In addition to the involuntary experiences described above, a person with PTSD may experience an attack that requires rapid relief. It begins in response to some external stimuli, which in psychology are called triggers. They return the patient back to the past, to those terrible conditions. It could be noise, a bright flash of light, even a single word. The patient panics that now everything will happen again. The emotions experienced are so strong that it is no longer possible to cope with them on your own. At this moment, you can observe the so-called “emotional / somatic flashback” - a grimace of rage frozen on the face. Hysterics begin and inappropriate actions are taken. Being around such a person is dangerous. He can hit, push, cause damage.
Other symptoms
However, the symptoms are not limited to these three main signs of the disease (they are listed in ICD-11 as criteria for diagnosis). There are many accompanying markers.
Mental:
- increased anxiety, hypervigilance, suspiciousness;
- obsessions;
- nervousness, psychosis, outbursts of anger, attacks of aggression and anger (most often causeless);
- panic attacks, fears, phobias;
- sleep apnea, insomnia, nightmares;
- isolation, autism, desire for loneliness, severance of previous connections, social maladjustment;
- internal complexes;
- loss of interest in life, suicidal tendencies.
Physical:
- hyperhidrosis;
- tremor of the limbs;
- violation of speech and motor functions;
- rapid and uneven breathing, shortness of breath;
- dizziness, fainting;
- hyperemia or vice versa - excessive pallor of the skin;
- gastrointestinal disorders: nausea and stool disorders;
- ringing in the ears, fog and spots before the eyes;
- tachycardia, heart failure.
The cognitive sphere also suffers: inability to concentrate, distracted attention, memory problems, inhibition of thought processes.
A distinctive feature of PTSD is that it may not reveal itself immediately after a psychological trauma, but several months and even years later. The trigger is usually a trigger; the disease begins unexpectedly and progresses incredibly quickly. There are cases where symptoms among participants in combat operations made themselves felt 40 years after the end of the war.
Relatives in whose family there is a person with this diagnosis need to know when and how post-traumatic stress can manifest itself in order to help him. One of the components of successful treatment is counseling the patient’s relatives on what to do in such situations.
Risk factors
There are certain factors that increase your risk of developing PTSD. These include:
- character accentuations;
- sociopathy;
- mental development below normal;
- chemical dependencies;
- history of mental disorders (genes);
- existing traumatic experience;
- children or old age;
- difficult socio-economic situation of an individual, family, society;
- isolation at the time of experiencing trauma;
- inadequate reaction of the environment (sick reactions are encouraged) and late or incorrect help.
In general, the development or non-development of PTSD is influenced by how subjective and objective the threat was; how close the person was to the center of events; how loved ones reacted and were involved. The latter is especially important for children: the reactions of children largely depend on the reactions of their parents.
A traumatic situation is one condition for the development of PTSD, another condition is the corresponding characteristics of a person’s inner world, reactions to trauma, which are individual in each case.
Stages of PTSD
In clinical psychology, it is customary to distinguish 3 stages of the disorder: acute PTSD, chronic and delayed.
Acute stage
Up to 6 weeks after the traumatic event. Man is driven by fear. The perception of time and reality, space changes, the person suffers from excessive activity or falls into a stupor. Among the physical manifestations:
- uneven breathing and rapid heartbeat;
- sweating;
- nausea;
- sudden short movements (jerking);
- hand tremors;
- tinnitus;
- stool disorders;
- fainting, headaches and dizziness;
- decreased concentration;
- sleep disorders.
At the emotional level, there is a feeling of helplessness, hypervigilance and outbursts of anger, accusations, fear, guilt, anticipation of danger, constant anxiety and reliving the situation.
The nature of the development of symptoms depends on individual personal characteristics: they will weaken or intensify, disappear or not. At this stage, debriefing (a conversation between a psychologist and a person who has suffered psychological trauma) and hypnosis are indicated. If help was not provided or was incorrect, then the next stage begins - chronic.
Chronic stage
From 6 weeks to six months. There are behavioral disturbances due to anxiety about the future life and a feeling of uncertainty. At this stage, it is important to talk about the problem, express your thoughts and feelings. If this does not happen, then anxiety intensifies, a thirst for revenge and aggression develops.
The main characteristic feature of the stage is depression combined with constant severe fatigue. Memories come up on their own. The person becomes fixated on the trauma, relationships with loved ones deteriorate, and the quality of life suffers. The victim finds himself cut off from reality; he cannot perceive it adequately.
As a result, a person chooses for himself some form of escape from reality. The way to help at this stage is psychotherapy. If help is not provided, then the delayed stage begins.
Delayed stage
From six months to several years after the traumatic event. All the symptoms described in the next paragraph are observed. Depression and addictions are getting worse. A person completely loses control over his own life. Tries to “revive” himself with other strong shocks.
Symptoms of PTSD
Several groups of symptoms are observed.
Dissociative symptoms
- Traumatic images themselves emerge.
- Constant thoughts about what happened.
- Feeling of emotional dependence.
- Staying “here and there,” that is, wherever a person is, he simultaneously seems to be in that traumatic situation all the time.
With each uninvited memory, the person again experiences extreme stress. Sometimes he may even perform involuntary defensive actions, such as falling to the ground.
Trauma reminds you of itself in a dream. This may be an exact reproduction of what happened or a variation. Just as events can repeat themselves identical to reality, a person in a dream relives his emotions.
From such dreams, the victim wakes up tired, sweating, muscles are stiff, and the heart is working at the limit. Naturally, the quality of sleep suffers because of nightmares (fear of falling asleep, trouble falling asleep, early awakening, restless sleep). Fatigue and apathy gradually accumulate.
Symptoms of Avoidance
The personality tries to repress any memories of the traumatic event:
- avoidance of thoughts and memories of the experience;
- avoidance of situations reminiscent of the experience;
- avoiding people, places, conversations that may remind you of the trauma;
- forgetting the most important moments of a traumatic situation;
- a person becomes absolutely apathetic and indifferent to everything, even what previously aroused great interest;
- there is a feeling of loneliness and detachment.
Gradually, the individual partially or completely loses the ability to establish close relationships with people. Emotions and feelings such as love and joy become inaccessible due to defensive emotional stinginess.
Creative potential is noticeably reduced. Along with this, the feeling of alienation from the entire world around us increases. The person himself feels that he is moving away. Based on the changes, a new self-image is formed. But it is difficult to express these feelings and sensations, as a result of which the individual, with the thought that no one understands him, actually withdraws into himself.
In turn, against the background of “they don’t understand me,” depression, self-doubt, and a feeling of worthlessness and uselessness develop. The meaning of life is lost, apathy and exhaustion develop. Often a feeling of guilt and an orientation towards a short life is formed, self-destructive behavior or aggression towards the outside world is noted. If a person abuses alcohol, then outbursts of anger become brighter and more unexpected.
Physiological hyperactivity
These are different types of reactions of the body:
- insomnia;
- irritability;
- decreased concentration;
- outbursts of anger and other affective reactions;
- hypervigilance;
- readiness to "run".
Symptom #3: Avoidance
A girl with post-traumatic stress disorder (PTSD) at an appointment with a psychologist
Our brains want to stay away, very far away from anything even remotely related to the trauma we experienced. If you are attacked in a parking lot one night, you will avoid parking lots. Car accident survivors often never drive again. Victims of burglaries move to another apartment.
Avoidance is not limited to physical movement, it includes thoughts, memories and emotions. For example, many survivors are unable or unwilling to talk about what happened. Others stop trusting others.
You may avoid strong emotions, being unable to experience feelings of love, affection, tenderness, sexual desire, or sadness, loss and grief.
Avoidance often takes the form of using alcohol or drugs to block out overwhelming feelings.
Avoidance has far-reaching goals. To feel safe, the brain builds a huge protective wall, regardless of the price it has to pay for it.
Claire, a 20-year-old student, was attacked by her boyfriend while she was sleeping. After this, Claire lived for years, afraid to fall asleep, because she did not consider herself safe. This concern was justified given her experience.
She worked double shifts, studied at night, and lived on caffeine, a lifestyle that surprised no one in our workaholic society. It was only after she fell asleep at the wheel one day that Claire decided to seek help.
WORKER POLYGRAPH PROTECTION ACT OF 1998 USA
Types of People Suffering from PTSD
PTSD affects up to 1% of people and up to 15% of people who have experienced severe trauma. Often the disorder becomes chronic and is combined with other diseases. There are several types of people based on how trauma has affected them and what kind of help they need.
- Compensated people who have enough support from their close circle.
- Mild maladjustment. Such people need both the support of loved ones and the help of a psychologist or psychotherapist. The existing imbalance can be easily eliminated with timely and correct assistance.
- Disadaptation of moderate severity. You need the help of family, friends, a psychologist and, as a rule, a doctor. Predominant emotions: anxiety and fear.
- Severe maladjustment. Long-term treatment and recovery are required. The list of assistants is selected individually, according to the injuries received.
PTSD in children
Children endure any stress more acutely. The range of critical situations is also changing. A traumatic situation for a preschooler can be separation from a parent or communication with a stranger. For a school-age child - failures in school or relationships with peers.
Instead of escaping reality, regression of behavior is more often noted as a reaction to trauma. The rollback depends on the initial development, but anything is possible: enuresis, thumb sucking. The remaining symptoms are the same, mainly fear and anxiety, psychosomatics. Another question is that the child cannot always tell about his condition. Parents must be especially vigilant.
PTSD can affect a child’s physical and mental development and cause delays. Defense reactions include aggression and isolation.
Children cannot always connect the experienced event and their feelings. That’s why they can see dreams simply as nightmares and express their thoughts unclearly. Until the age of 10-13, it is better for parents to describe what happened.
Children experience PTSD in 5 stages:
- Despair. It manifests itself as acute anxiety in response to what happened and a lack of understanding of what happened.
- Negation. Insomnia, withdrawal reaction, memory impairment, disinhibition, and psychosomatic reactions occur.
- Obsessiveness. There are sleep disturbances, fear, constant emotional arousal, and instability of emotions.
- Working through. The child realizes what happened, the reasons for it, mourns and works through it.
- Completion. There are hopes for a new bright future. The ability to make plans for the future returns.
Diagnosis of PTSD
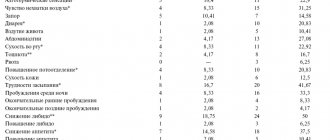
To diagnose the acute stage of PTSD, observation by a specialist is sufficient. At later stages, it is necessary to conduct diagnostic tests, techniques for assessing PTSD itself and for identifying and assessing disorders. There are a huge number of them, I will name a few.
- SKID – structured clinical interview for diagnosis.
- PTSD Clinical Diagnostic Scale (symptom identification).
- Dissociation scale.
- Spielberger-Hanin questionnaire to assess the level of anxiety.
- GTO – Traumatic Stress Questionnaire (I. Kotenev).
To identify personality disorders:
- Minnesota Multidisciplinary Personality Inventory (Mental Disorders).
- Luscher color test (reveals unconscious anxiety and psychological discomfort).
- SAN – assessment of well-being, activity, mood.
- Rokeach's test of value orientations.
- Any tests for anxiety, aggressiveness, depression.
Correct diagnosis is a very important element. Therefore, you need to entrust this to a professional. It is important to correctly arrange the methods, choose one or more. It is possible that additional methods will be needed, for example, self-diagnosis tests.
For children, it is better to use conversation, color test and projective techniques. Or display the PTSD index. To do this, you need to answer the following statements:
- The event is perceived as a strong stress factor.
- The child becomes upset when thinking about the event.
- Afraid of a repeat event.
- Gets scared when thinking about the event.
- Avoids anything that reminds you of the event.
- Excited (nervous) gets scared easily.
- Wants to avoid feelings.
- Obsessive thoughts.
- Bad dreams.
- Sleep disorders.
- Intrusive images and sounds.
- Loss of interest in previously significant activities.
- Difficulty concentrating.
- Detachment (increasing interpersonal distance).
- Thoughts about the event interfere with studying.
- Guilt.
For each positive statement, a point is awarded. 7-9 points indicate a mild degree of PTSD, 10-11 - moderate degree, 12 and above - severe.
Symptoms of Post-Traumatic Stress Disorder
A specific sign of this syndrome is the presence of intrusive memories of the event that caused psychological trauma. Such memories are characterized as unusually vivid, but in the form of fragments - pop-up pictures from the past. In most cases, the appearance of these images is accompanied by a strong feeling of constant alertness, melancholy, horror, and helplessness.
An attack of negative experiences entails changes in the functioning of the autonomic nervous system, manifested in the form of increased blood pressure, changes in heart rate, excessive sweating, and frequent urination.
Some patients experience a feeling that the past is coming back to life. These people tend to form illusions that involve a pathological perception of external stimuli. Visual and auditory hallucinations may also occur. Such manifestations provoke aggression, inappropriate actions, and suicide attempts.
In addition to intrusive memories, people who have experienced severe mental trauma are characterized by the following conditions:
- excessive vigilance;
- high level of anxiety;
- paranoia;
- neurosis;
- depression;
- sleep disturbance;
- emotional coldness;
- difficulties in thinking processes, memory and attention.
The patient cannot tolerate loud sounds, darkness and other factors accompanying a traumatic situation. Some people may start using alcohol or chemicals in an attempt to forget the sad event.
Correction of PTSD
The main method of treatment is psychotherapy. It needs to start with normalization, that is, with a discussion of the feelings and emotions of the victim and their normality. It is important to establish a partnership with the victim, and to do this, take into account his vulnerability, low self-esteem and vulnerability. It is also important to take into account the individuality of each person and the varying course of PTSD.
The more time has passed since the injury, the more difficult the work will be, since PTSD is already closely woven into the personality structure and other psychological problems. Psychotherapy can take from one month to several years. If a person has maintained relationships at work and at home, and has a positive attitude towards psychotherapy, then the prognosis for correction is good. Otherwise - unsuccessful. But you can never say for sure.
Work with the victim is carried out in the following areas:
- correction of self-concept;
- formation of objective self-esteem;
- regaining self-confidence;
- restoration of the system of needs and values, including their hierarchy;
- correction of claims and expectations (with a focus on current psychophysiological capabilities);
- the return of empathy, the establishment of relationships with others, the return of the ability to establish close relationships;
- mastering the science of conflict prevention and resolution, developing communication skills;
- eliminating depression and unhealthy lifestyle.
Within the framework of therapy, 4 types of methods are usually used:
- Educational awareness. To destroy the myth of the uniqueness of what happened and loneliness in the problem, it is necessary to familiarize the victim with books, articles, television shows, scientific theories, classifications and international clinical symptoms of PTSD.
- Promoting a holistic healthy lifestyle. Description of its significance for recovery from PTSD.
- Social rehabilitation, that is, the active inclusion of a person in society: group and family therapy, rehabilitation centers.
- Psychotherapy itself, broken down by each of the identified issues (fear, grief, depression, psychosomatics, etc.).
Within the framework of psychotherapy, the most popular and effective are 3 methods.
Desensitization and eye movement training
The method cannot be used by untrained people or non-professionals, as it can harm the victim. Rapid eye movements activate a psychophysiological mechanism that processes and adapts stress information. With PTSD, the trauma seems to be frozen and the mechanism is blocked. Eye movements activate it and release the trauma. The number and duration of sessions is selected individually.
Visual-kinesthetic dissociation
Refers to NLP techniques. The technique assumes that the victim has hidden resources. It is necessary to transfer them from a subconscious level to a conscious one and teach them how to handle them. The procedure involves viewing the traumatic situation and installing anchors in safe places. A person seems to look at himself from the outside: in prosperous and traumatic situations. The event of trauma and the negativity from it is placed between prosperous memories.
Mitigating a Traumatic Incident
Involves reliving the trauma under the supervision of a specialist. This can be viewing frames, photographs - in general, any visualization. The point is that there is a rethinking, a revaluation of the trauma. An important condition is the provision of a safe space by the therapist and the consent of the victim to the procedure, his openness. It's just viewing. Commenting, rating, and discussions are excluded. You need to go through the path again from beginning to end without stopping. The viewing is repeated until the victim can look at it calmly.
These are not all the methods that can be used. Psychological debriefing, other NLP techniques, Gestalt therapy, support group, group therapy, family and marital therapy, hypnosis, and art therapy are also used. When selecting correction methods, the nature of the injury must be taken into account. For example, when experiencing grief or potential suicide, the correction program will be completely different.
Treatment of PTSD
- Cognitive behavioral therapy involves teaching skills to help the patient change their negative thought processes. It also involves mental images of the traumatic event to help overcome the trauma to gain control over fear and distress.
- Exposure therapy involves the patient safely confronting what upsets and worries him so that he can learn to cope effectively with it. But some experts point out that it may actually do more harm than good.
Medications
- SSRIs
(selective serotonin reuptake inhibitors) are the most commonly prescribed medications for PTSD.
An example of such a drug is paroxetine
. It helps treat depression, anxiety, and sleep problems—symptoms often associated with PTSD. - Benzodiazepines
are effective in treating irritability, insomnia, and anxiety. They should be used with caution because they can be addictive. - Ecstasy
, the pharmaceutical version of ecstasy, helps patients deal with memories effectively. - Hormone therapy with cortisone reduces the risk of PTSD.